Shane Hemphill, MD
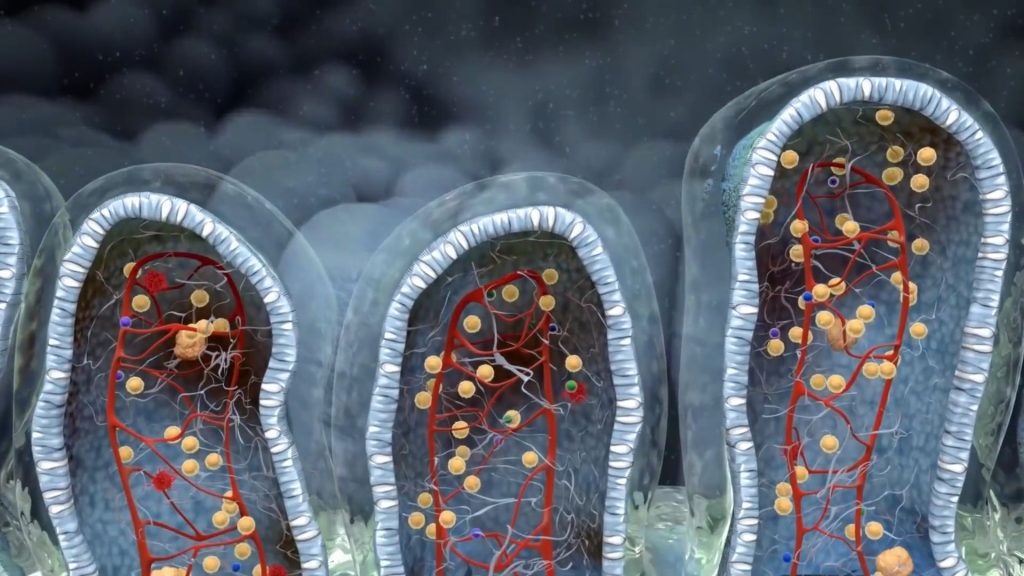
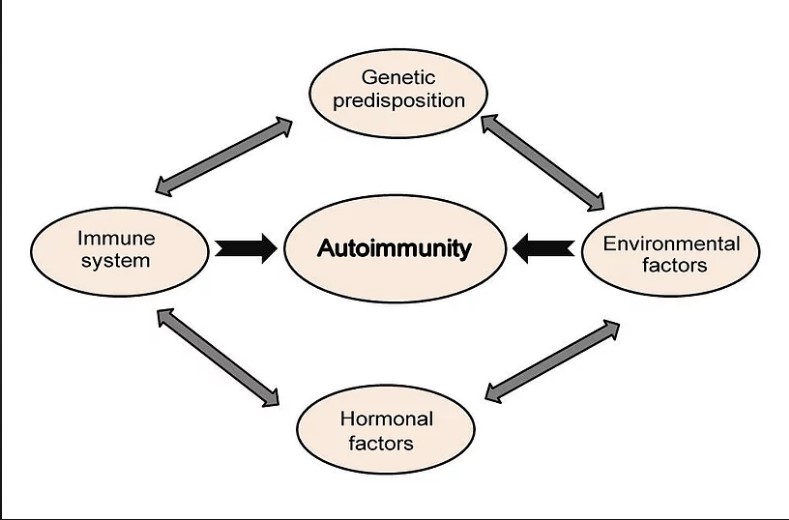
| Say your functional medicine provider ordered a stool test and it showed Low SIgA- what does that mean and how did it develop? The immune system makes T cells and B cells. The B cells produce secretory IgA (SIgA) which acts as a first line of defense against the entry of foreign substances into the body. These foreign substances include many things such as undigested proteins from the foods that we eat, bacteria, viruses, parasites, or even molds. In essence SIgA gives us insight into what is happening at our mucosal surfaces. The body’s mucosal surfaces – located at the eyes, ears, nose, throat, sinuses, gastrointestinal and genitourinary tracts, and skin are all entry points for potential disease-causing pathogens. Our body’s way of protecting these entry points is done with the release of SIgA. B-cells present within the mucosa are activated upon exposure to pathogens and allergens and thus produce SIgA in response. The SIgA then attaches itself to the invading bacteria, virus or other foreign substance, traps it in the mucosal surface and then neutralizes it. So what does it mean if your SIgA is low? If your SIgA is low, this means that you are less able to prevent invaders from getting into your gut mucosal lining. This lining can become inflamed and tight junctions that ordinarily keep toxins and undigested food particles out – break down. This causes havoc as now toxins and undigested substances are able to get access to our blood stream, causing inflammatory and immune reactions that lead to systemic symptoms throughout the body. Patients with low SIgA levels generally have increased risk of food sensitivities, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), intestinal permeability also known as ‘leaky gut’, autoimmunity, and other gastrointestinal infections. What causes low SIgA levels? Chronic infections are commonly associated with low SIgA. Assessing for problematic bugs including H pylori, Candida, Blastocystis Hominis, H. Pylori, Clostridium difficile are essential in this evaluation. Do keep in mind that many of these normally can exist in the bowel at low levels and not cause harm. Some of them only become problematic depending on their level in the body and others do it based on virulence. These can be assessed via a functional stool test. One interesting note is that these ‘infections’ are opportunistic by nature, meaning they also come about when SIgA levels reduce. Therefore it is not uncommon to see development of Candida in SIgA compromised clients. Medications are another cause of low SIgA. Anti-inflammatories, antibiotics and antidepressants are some examples. Studies have even shown an association between low SIgA and people that suffer from depression. Stress is another cause of low SIgA through increased cortisol levels. Stress can be in any form, including mental, emotional or even physical. One study has even demonstrated that persistent negative thoughts about ourselves can lower our own SIgA levels. Lowering stress and introducing stress reduction techniques is vital in maintaining this protector. Finally, poor dietary choices are another contributor to low SIgA. Certain nutrients such as Vitamin D, Vitamin A, Zinc and Glutathione are instrumental in supporting healthy SIgA levels. A good intake of dietary fiber and phytonutrients can also play a role in supporting a healthy gut microbiome. This can lead to the development of beneficial bacteria that promote healthy levels as well. Stay tuned for my next article which will discuss how we treat low SIgA. To schedule a new patient appointment, please call our office at 919-999-0831. Your Partner in Health! Shane Hemphill, MD |
 |