
Disrupt Negative Thinking Through The Power Of Gratitude

 919-999-0831
919-999-0831

Clarissa A. Kussin, ND, FMCHC, ERYT-500
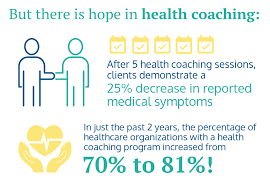
New Year’s is the time when everyone is looking toward the year ahead and all that they want to achieve. While people make resolutions with the best of intentions, few follow through and achieve their goals. This is where health coaching comes in handy.
Health coaches help support clients as they work toward making sustainable lifestyle changes. They are passionate about helping others live happier and healthier lives. This includes helping them stick to New Year’s resolutions. Whether you want to reduce stress, eat better, or move more, health coaches can guide the way.
The Power of Personalized Guidance:
A health coach is your dedicated partner on your wellness journey, offering personalized guidance that goes beyond generic advice. They work with you to create a tailored plan based on your unique needs, preferences, and health goals.
Medical Benefits of Having a Health Coach:
How to Get Started:
If you’re ready to experience the transformative benefits of health coaching, reach out to us today! Our team of experienced health coaches is here to guide you on your journey to optimal health. Call 919.999.0831 to get scheduled.
Remember, investing in your health is an investment in a brighter and more fulfilling future.
To your health and happiness!
References:
Wing, R. R., et al. (2018). Intensive lifestyle intervention in type 2 diabetes. New England Journal of Medicine.
Ockene, I. S., et al. (2007). The role of counseling in the promotion of healthy behaviors in adults. JAMA.
Huffman, J. C., et al. (2018). The role of stress and psychosocial interventions in cancer. Current Psychiatry Reports
Warburton, D. E. R., et al. (2006). Health benefits of physical activity: the evidence. Canadian Medical Association Journal
Your Partner In Health,
Clarissa A. Kussin, ND, FMCHC, ERYT-500

Frances Meredith, MD

| Concussion is so much more common than we realize, a frequent occurrence in kids and teens, especially athletes, and increasing frequency in the elderly and unstable of gait. The fact that memory loss can be associated creates a scenario where concussions are simply not recalled, but can lead to long lasting symptoms and deterioration in quality of life. Most people do not seek care, and when they do, they are usually given out dated advice unless seen at a dedicated concussion center or provider. Sadly, most medical professionals, even in an urgent care or ER, are not trained in current cutting edge acute concussion care. Concussion centers have only come into existence since 2000, and active research has been lacking until recently. What is very clear is that with any symptoms suggestive of concussion (including loss of consciousness, dizziness, or feeling “detached”, vision changes, headache, nausea), physical activity must stop immediately. Theon field symptom that best predicts a longer recovery is dizziness followed by “fogginess”. Estimates according to Dr Michael Collins, head of the concussion center at UPMC University of Pittsburgh Medical Center, are that for every minute a player is back on the field, his/her recovery time is lengthened by7-8 days (1). The average recovery time for a mild concussion is 18 days, with15 minutes back on the field prolonging this to 44 days. What is not widely recognized is that immediate evaluation, a graded exercise and brain rehab plan, and supplement support can greatly speed recovery. EVALUATION An evaluation by a doctor familiar with concussion is essential after head trauma. Assuming the doctor feels you can be monitored at home, someone should stay with you and check on you for at least 24 hours to make sure symptoms are not worsening. This should be followed be evaluation by a true concussion expert as soon as possible. Evaluation should include an assessment of the mechanism of injury itself(video very helpful if available), vestibular ocular motor screening, balance and autonomic nervous system testing, and can include more sophisticated testing including a qEEG brain scan and Right Eye testing. An assessment of preconcussion risk factors which might delay recovery is important as well as a determination of the type of concussion. There are, according to current research, six types of concussion: cognitive fatigue, vestibular, ocular, migraine, anxiety, and neck based. These can overlap, and these different types are treated with different therapeutic modalities guided by testing. MANAGEMENT Mental rest and eye rest are essential in the early days after concussion. How long you’ll need to rest your brain and body will depend on the severity of your concussion and rapidity of resolution of symptoms. Your concussion specialist will help you to create a plan to allow the brain to heal. This will include lots of rest, optimizing hydration, and initially completely avoiding activities requiring mental concentration including homework, watching TV, playing video games, texting and using computers. These activities should be avoided for at least the first 48 hours after concussion, then gradually brought back incrementally as tolerated. Physical activity should also be limited in the first few days to mild activity such as walking that does not trigger symptoms. At that time exercise becomes essential in the healing process. Previously recommended complete bedrest, in darkness avoiding all stimuli, is no longer recommended. A structured, gradually progressing exercise plan should be created with your concussion specialist. Exercise programs after concussion often consist of 45-90 min daily of intense activity to increase blood flow to brain. Exercise is the best way to increase Brain Derived Neurotrophic Factor (BDNF), essential in neuroplasticity and brain healing. Optimal sleep is essential, with experts recommending at least 8 hours nightly with consistent bedtime and awakening times, taking only short naps when needed during the day in order to ensure optimal nighttime sleep. Your doctor may recommend, as screentime and mentally focused activities are reintroduced, a lightened work/school schedule, and spacing out screentime such as homework in short blocks. Your doctor will likely recommend other modalities to “rebab” the brain including a combination of exercises for vision and balance, Neurofeedback, autonomic nervous system retraining, and laser therapy. Often chiropractic care will be advised to reestablish alignment in the neck as misalignment in the neck gives the brain incorrect information about where you are in space. For pain relief discuss with your doctor whether Tylenol is right for you as NSAIDS such as Ibuprofen or Aspirin can increase risk of bleeding and actually prolong inflammation. As the brain is working hard to clear out damage, it is essential to abstain from other toxins to the brain such as alcohol, and lay off cigarettes if you smoke. “Energy Crisis” Optimal nutrient support at the onset of concussion may have an impact on speed of recovery. To understand why, it is key to understand what is happening in the brain in the minutes after concussion. The brain depends on glucose for energy. Following concussion, an “energetic crisis” occurs in the first 24 hours after injury where the brain can no longer easily metabolize glucose. Just when the brain needs more energy to heal, it has much less. This is followed by neuroinflammation at the site of injury that can further impair metabolism and energy production in the brain. Neuronal damage is also accompanied by vascular damage in which the pumps that keep nerves stable begin to fail. Then glutamate, a neurotransmitter toxic when in high amounts, can leak out and create inflammation and cell death. The goal is to decrease energetic demands on the brain and provide an alternate source of fuel other than glucose: ketones. Ketones serve as an alternate fuel source for the brain, typically created from fat stores while fasting. There is limited research in this area but animal studies are supportive and human studies are ongoing. The mechanisms of injury above guide treatment options that can be helpful in the hours to days after concussion. These can include: –Ketogenic diet: Ketones created in a low carbohydrate “ketogenic diet” support brain energy and can be supported by “exogenous ketones” in powder form. Studies in rodents show therapeutic benefit(4,5); studies in humans are lacking and ongoing but safety of ketogenic diet has been established. –Anti-inflammatory nutrients and anti-inflammatory diet: Nutrients such as fish oil, DHA, Vitamin D,NAC, Vit C, and curcumin have growing research to support their therapeutic benefit. –Phospholipid Support: Phospholipids, the main component of cell membranes, are made up of fats and phosphate. Studies suggest phospholipid support can help repair a damaged blood brain barrier and reduce tissue damage with traumatic brain injury (TBI)(8,9) –Hyperbaric oxygen treatment: Research suggests hyperbaric oxygen may be beneficial in both acute and chronic concussion or CTE (chronic traumatic encephalopathy) (6,7) however more research is needed. As the research grows, our approach to concussion will be fine tuned in the years to come. Please spread this information to family and friends as this knowledge can be the difference between return to play with speedy recovery and a lifetime of frustrating neurologic and psychologic symptoms that can be the result of poorly managed concussion. With expert management, top practitioners in the field firmly believe that complete healing is possible. Your Partner In Health, Frances T. Meredith, MD |

Sara Yadlowsky, FMHC
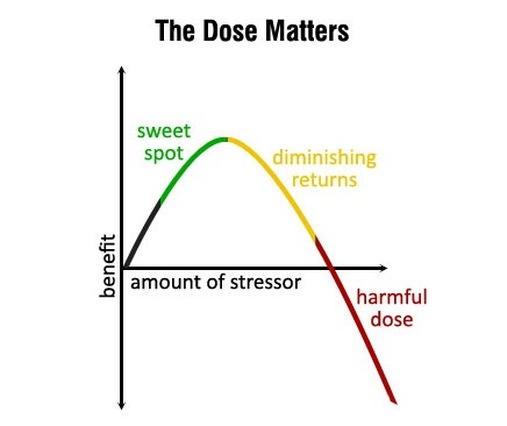
What doesn’t kill you makes you stronger. We’ve all heard the saying before. Science has revealed it is surprisingly accurate when it comes to our health and longevity.
Hormesis is the idea that short, intermittent bursts of certain stressors can start a cascade of cellular processes that slow aging, improve overall health and make you more resilient, both physically and mentally. It is a hot topic in longevity research right now.
We all know that chronic stress caused by relationship issues, financial problems and working too many hours is detrimental to our health. However, hormetic stressors are controlled and acute, triggering healthy adaptive responses.
What does all this mean in real life? Hormesis is the common thread found in some popular health and fitness trends such as HIIT (high intensity interval training), cold exposure, heat therapy and intermittent fasting. Prolonged doses of these behaviors are not healthy or sustainable. For example, if you spend too much time in a sauna you will become dehydrated. But, in short bursts, the bodily stress caused by these practices are enough to bring about health benefits such as reducing inflammation, supporting elimination of toxins, repairing DNA, combatting oxidative stress, repairing cellular damage and reducing risk of cancer.
Here are three ways to strategically stress your body and reap the rewards:
Be aware that adding stress (even the good type!) to our lives can backfire if done at the wrong time. When life is already very stressful, it is best to wait until a better time when you are more relaxed to try out these new practices.
Your Partner In Health,
Sara Yadlowsky, FMHC
Susan Denny, MD, MPH
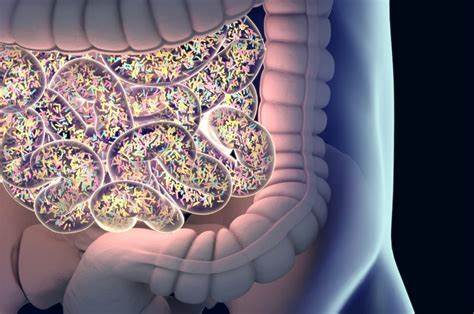
Do You Have Leaky Gut?
If you suffer from a chronic health condition and have been researching how to improve your health, you may have heard of leaky gut. If that conjures up an unpleasant image of gut materials leaking in to your bloodstream, you are not far off. Leaky gut happens when contents from the small intestine spill into the sterile bloodstream from a damaged or “leaky” gut wall. This contamination of the bloodstream by digested foods as well as bacteria, yeast, and other pathogens is often the foundation for chronic inflammatory and autoimmune health disorders.
Leaky gut is referred to as increased intestinal permeability in scientific research and is increasingly being recognized as a common underlying factor in most inflammatory symptoms and disorders. As our body’s largest immune organ, the gut powerfully influences the rest of the body. Importantly, this includes the brain. Current scientific studies link intestinal permeability with inflammatory bowel disorders, gluten sensitivity, celiac disease, Crohn’s disease, type 1 diabetes, depression, anxiety, psoriasis, and many other chronic conditions.
Given what we know about the connection between gut health and immunity, it is vital to include a gut repair protocol in the treatment of inflammatory and autoimmune disorders. Repair of leaky gut begins with understanding why it developed in the first place. Reasons for leaky gut can include over the counter or prescription medications, antibiotic use, toxin exposure, hormonal changes, food intolerances, poor diet and others. After root causes are identified, a leaky gut protocol can help you improve your health, relieve symptoms, boost energy, make you happier, and clear your brain fog. Ask our office for advice on improving your overall health through a personalized leaky gut evaluation and treatment plan.
Your Partner in Health!
Susan Denny, MD, MPH
Erica Nelson, MSPH, NBC-HWC
They say the mind is a wonderful servant but a terrible master. Are you in charge of your mind and body? Or do you feel like you are at the mercy of your thoughts and feelings (physical and emotional)? This article shares cost-free and drug-free practical strategies to take back control of your physical and emotional feelings and make your mind your servant.
Your nervous system is complicated but you do not need to know all of the details to have a significant impact on its function. In this article you will find a very simple description of how one specific nerve, the Vagus, connects your physical and emotional feelings. You will also learn practical things you can do to reduce anxiety, improve digestion and overall wellbeing.
Starting from the top, the brain branches out from your skull through 12 cranial nerves (and their branches) known as the peripheral nervous system.

Starting from the ‘bottom’ the gastrointestinal ‘mind’ is called the enteric nervous system (ENS.) The ENS has more nerve cells than the rest of the entire nervous system combined (more than 100 million!) and is capable of functioning independently of the rest of the nervous system.
The Vagus nerve is one of the 12 cranial nerves. It connects your brain to your digestive system and vice versa. It sends and receives both motor (movement) and sensory (feeling) signals. Beyond the digestive system, it touches nearly every major organ and plays a role in heart rate, respiration, facial expression, inflammation, sweating, reproduction and more.
Photo courtesy:
www.drarielleschwartz.com

The word ‘Vagus’ comes from the Latin for ‘wander’ but, as Tolkien wisely said, ‘Not all who wander are lost.’ This nerve, and its branches serve as the information super highway in your body and provide the early warning system for threats, internal and external.
Most of these functions are reflexes that happen without you thinking about them to keep you alive. Can you imagine if you had to decide to shunt blood supply from your stomach to your heart and lungs to run from danger? But sometimes the reflexes are not actually helpful in the moment and we are left feeling like our stomachs have minds of their own – because they kind of do. But when we know what the reflexes respond to, we can take steps to trigger a more desirable response.
Toning the Vagus for Stress Resilience
Have you ever felt your mouth go bone dry just as you are about to begin a presentation or performance? Or worse, maybe you feel like you are going to throw up? Or need to go to the bathroom RIGHT NOW. This is your reflexive response to stop bodily secretions and smooth muscle contractions in your GI tract so you can spend your resources elsewhere.
When you perceive a threat, your brain and body make preparations to respond and additional resources – oxygen, fluids, etc. – are diverted from digestion and reproduction until you are physically and psychologically safe again. Your heart rate, blood pressure and breathing increase, your pupils dilate, your mouth may go dry, your muscles may begin to tremble all of these are signs of activation of your sympathetic nervous system.
It is the job of the parasympathetic nervous system, including the Vagus nerve, to restore resources to ‘rest and digest’ once the threat (perceived or real) is passed. Depending on the duration and intensity of the threat, it may take 20 minutes or 20 years to return to a healthy resting state. When left unattended, chronic stress or PTSD can have long-term effects on your physical, cognitive and emotional health.
This exercise lengthens and contracts the Vagus nerve to activate it. Get on your hands and knees on the floor. Begin with a neutral spine and then press down through your hands and knees to arch your back upwards like a cat. Inhale while doing this. Then drop your belly down towards the floor and lift your breastbone forward and up. Exhale loudly while you do this, sticking your tongue out and even roaring like a lion.
Laughter really is one of the best medicines. Real laughter is best but even fake laughter will engage the Vagus nerve through contraction of the diaphragm.
A warm embrace, ideally 20 seconds or longer, will stimulate the part of the Vagus nerve that runs down your back and can trigger the release of a hormone called oxytocin, known as the feel-good hormone.
The Vagus nerve is connected to your vocal cords and the muscles at the back of your throat. All of these activities activate the muscles around the nerve and can stimulate it. Choose one or more and find time for it each day.
Place the tip of your tongue against the ridge of tissue just behind your upper front teeth, and keep it there through the entire exercise. Exhale completely through your mouth, making a whoosh sound. Close your mouth and inhale quietly through your nose to a mental count of four. Hold your breath for a count of seven. Exhale completely through your mouth, making a whoosh sound to a count of eight. This is one breath. Now inhale again and repeat the cycle three more times for a total of four breaths.
This works for a couple of reasons. First, when you are walking, your eyes naturally move side-to-side and trigger a response in your brain that distracts it from threat. Second, you are using up some of the ‘energy hormones’ that were dumped into your system to respond to the threat and may be making you feel ‘jittery.’
Stroke your neck from your ear to your clavicle 10 times on each side. Again, your Vagus nerve is connected to these muscles. Moderately intense massage to the area will stimulate the nerve and help to restore a resting state.
You do not have to be at the beck and call of your body’s reflexes. Choose one or two of the strategies above and integrate them into your day to improve your ability to respond the way you want to – instead of simply reacting – the next time you are faced with a stressful situation.
Call our office and schedule an appointment with one of our health coaches to learn more healthy strategies to reduce and respond to physical, emotional and cognitive stress.
Your Partner in Health!
Erica Nelson, MSPH, NBC-HWC

Sara Yadlowsky, FMHC

Summer is in full swing, which means weekend getaways and road trips. While for some a trip to the beach can help deter the stress associated with day-to-day life, for others it might spark a pang of anxiety. One of the most common questions we get as the weather gets warmer is: “how do I stay on track with my wellness goals while I am on vacation?” For so many of us, the excitement of being on a much-needed vacation coupled with an environment of food options that we do not usually indulge in creates a perfect storm of bloat, fatigue and overall unhappiness.
Here are some tips on how to stay on track while on vacation while still be able to enjoy yourself.
Bring Along Some Food From Home
Stay on track with your diet by bringing some food from home. Whether that mean fresh veggies and fruit, gluten-free bread, your favorite protein powder or organic meat, make sure that you are sticking with your routine from home to not only encourage healthy eating while away, but also to avoid temptations of food items that may cause unpleasant side effects.
Drink Lots of Water
Drinking lots of water daily is critical to your wellbeing and it’s even more important while you’re on vacation. Making sure that you are staying hydrated can help aid in digestion and prevent constipation while you are traveling. If you are indulging in alcoholic beverages while on vacation, this tip is even more crucial. It’s an excellent idea to alternate between alcohol and water in order to avoid dehydration.
Prioritize Whole Foods
Eating an adequate amount of vegetables and fruit while on vacation will keep your fiber intake up during vacation. An easy way to get lots of whole foods is to make a superfood green smoothie for breakfast with plenty of fruits and veggies added in. Continue to prioritize whole foods throughout the day by getting veggies and/or fruits at every meal.
Get Plenty of Sleep
Being on a vacation always couples with being out of your normal routine; which is typically a good thing unless it interferes with your sleep. As tempting as it is to stay out later, getting a couple hours of sleep in before midnight will provide you with enough restorative sleep to help maximize your sleep and, in turn, stay on track with your wellness goals.
Don’t Stress
You’re on vacation after all! After navigating through the stress of daily life, this is your chance to lower your cortisol levels and spend quality time with loved ones. Don’t let your fear of losing traction on your goals interfere with your ability to truly enjoy yourself. If you backtrack a bit take it easy on yourself. Rather than beating yourself up for indulging in dessert the night before, celebrate yourself for going on a run the following morning.
Wherever your travels make take you this summer, I hope that these insights give you peace of mind to relish in the calm and come back feeling rejuvenated and ready to continue your wellness journey. Safe travels!
In health,
Sara Yadlowsky, FMHC
Blair Cuneo, PA-C
Lithium…a little goes a long way in cognitive and emotional health
Popular nutrients that make the major headlines for supporting cognitive wellness include magnesium and zinc, but how’s your lithium?
Lithium is an essential micro-nutrient with chemical properties similar to calcium and magnesium. It is present in all organs and tissues of the body.
The US Environmental Protection Agency estimates the daily lithium intake of an average adult ranges from 0.65 mg to 3 mg. Foods higher in lithium include grains, vegetables, eggs and milk. The most frequent source of lithium is tap water. Depending on where you live, there can be lithium deficiencies in your soil and with increased bottle water and home filtration use, we are filtering the lithium right out of our water.
Supplementing with low-dose lithium aims to support the body’s daily nutritional need for lithium. This is very different than the dosage of lithium as medication. Lithium carbonate is a well-established, effective medication therapy for mood disorders like bipolar disorder. Whereas lithium carbonate dosing can be in the hundreds of milligrams, low-dose lithium can range from micrograms to low milligram amounts.
How does lithium benefit brain health?
It is NEUROPROTECTIVE, shielding neurons from biological stress and toxins.
It promotes NEUROGENESIS, leading to increased numbers of neurons and brain volume.
It regulates NEUROTRANSMITTERS, helping to balance the mood.
Studies continue to accrue demonstrating improvement in mood and cognitive performance for patients with ADD, depression and Autism Spectrum Disorder. More recently, studies highlight the role lithium can play in prevention and treatment of Alzheimer’s disease, by inhibiting plaque formation and aiding in growth and repair of damaged neurons.
Screening for nutritional lithium deficiencies can be performed by hair trace mineral analysis, as blood testing is not sensitive enough to detect nutritional levels.
Talk with your functional medical provider about your cognitive and emotional health and find out if low dose lithium can further support your wellness goals.
Your Partner In Health!

Blair Cuneo, PA-C
Erica Nelson, MSPH, NBC-HWC
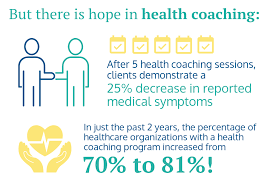
The legendary basketball coach, John Wooden once said, “A good coach can change a game. A great coach can change a life.” At Carolina Total Wellness, our coaches help our patients change their lives every day.Every patient at Carolina Total Wellness that sees a doctor or physician assistant is paired with a health coach. Some patients may also choose to work solely with a health coach to achieve their dietary and lifestyle goals. This article will help you know what to expect when you work with a health coach.
Here are 3 key aspects of the health coaching experience at Carolina Total Wellness:
The Space Between
Health coaches hold space for you to pause… and decide how you want to respond to your circumstances. The world today is a seemingly relentless onslaught of stimulation, and it can feel like there is an urgency to react to all of that stimulation.
George Mumford, meditation coach to Michael Jordan, LeBron James, Kobe Bryant and other world-class athletes offers another way, ‘Think about the eye of a hurricane.’ He says, ‘No matter how intense the storm or what’s swept up in its gale-force winds, that calm, blue center is always there. We all have this quiet center within us.’ Your CTW coach will help you respond from that quiet center within, rather than reacting from the chaos of the storm.
In our office, health coaches hold space for you to make sense of what is going on in your world and in your body and decide how you want to respond. Health coaches always honor the fact that you are the expert on your own life and display unconditional positive regard for you and whatever lifestyle decisions you choose. They pay attention to what matters to you and may offer suggestions for adjustments that fit into your life.
Translator
The science of the body and its systems are the physician’s expertise. Science of behavior change is the coach’s expertise. Our coaches help you translate medical science you discuss with your doctor or PA into evidence-based behavioral change strategies to optimize your health. When you combine the medical knowledge of our physicians and PA with your coach’s expertise in the science of motivation, habits, and change, many of the barriers to experiencing health fall away.
Each of the coaches at CTW has at least a bachelor’s degree from an accredited university and training in coaching from either the Functional Medicine Coaching Academy or Duke University. Some of them also have master’s degrees and other specialized training in nutrition, exercise, counseling, and other relevant fields. Unless otherwise specified, CTW coaches are not registered dietitians, licensed mental health professionals or certified fitness professionals.
Guide
In the words of Michael Jordan, ‘A coach is someone that sees beyond your limits and guides you to greatness!’ CTW coaches come to the table with empathy for whatever you are facing and feeling and confidence in your ability to overcome. Each coach has faced their own struggles in life and knows what it is like to work hard to overcome. However, coaches never replace you as the expert on you; they serve as your guide on your journey to health. Coaches can help you understand all the different ways you can try intermittent fasting or yoga or what, exactly, is ‘glycemic index.’ Maybe our most important job, though, is to help you get very clear on your vision of the healthiest version of you. Once you decide where it is you want to go, coaches provide education, support and accountability to knock down any stumbling blocks that may come up along the way.
Call us today to schedule your appointment with one of our health coaches.

Erica Nelson, MSPH, NBC-HWC
Didem Miraloglu, MD, MS
DO YOU KNOW HOW TO MEASURE YOUR WELL-BEING?

Ever heard of Heart Rate Variability (HRV)? Exactly as its name states, heart rate variability is a measure of the variability between heartbeats. Your heart beats a specific rate, anywhere from 60-100. There is a variation in this rate, depending on whether you take a deep breath, exercise, are under stress or are at rest. HRV is dependent on our nervous system to pick up cues from our environment. In order to understand how these cues are translated into physiological response, we first need to understand how the nervous system works.
Our nervous system controls our heart rate in two opposing directions.
One is the sympathetic nervous system, “fight or flight.” It is responsible for increasing the heart rate when we are stressed, like running away from a saber tooth tiger. In our present world since we are not normally faced with tigers, sympathetic drive kicks in during other emergency situations. This is exactly when you want more blood pumped from the heart to your muscles so you can fight or run. The blood pressure and heart rate increase as a normal response to the feedback from our environment.
Its counterpart is the parasympathetic nervous system, which is the “rest and digest” system. When our senses detect the emergency is all clear, our parasympathetic system takes the lead and tells our heart rate to slow down and lowers the blood pressure. Our body starts to relax.
This is the normal sequence of events that occurs by increasing and decreasing the heart rate appropriately according to the environmental cues. Studies have shown people with high heart rate variability are usually less stressed and are happier.
The problem occurs when there is low heart variability. This means the nervous system is not responding adequately to the environmental cues and hence your body is less resilient and struggles to handle changing situations. This may occur with diabetes, asthma, anxiety, depression and high blood pressure. This is also seen as we age.
You can improve your heart rate variability by taking care of your body and mind. Regular exercise along with a healthy diet, staying hydrated, avoiding alcohol, getting a good night sleep, being exposed to natural light, taking a cold shower and mindfulness, all help with reduction in HRV. Controlled breathing has also been shown to boost HRV and help fight stress which can decrease HRV.
The gold standard for measuring HRV is an EKG. But you don’t have to buy an EKG, since there are smaller and more affordable gadgets on the market with which you can measure HRV in the comfort of your home. Here are some of those:
There are also apps that help you increase your HRV. They do this thru teaching breathing techniques via biofeedback, which changes the heart rhythm to create a physiological balance in physical, mental and emotional systems. Some of these include HeartMate, HeartRate + Coherence Pro and HeartMath. HeartMath is the gold standard in the industry for coherence and the one with the most science behind it.
So, how do you measure your well-being? Mainly with tools that provide feedback on your heart rate variability. But remember, your well-being does not have so much to do with what is going on in your environment, as it does with how you perceive and react to your environment. And working on those factors will in long term help with your well-being.
“You have power over your mind – not outside events. Realize this, and you will find strength.”
Marcus Aurelius – Roman Emperor and Stoic philosopher (161-180 AD)

Didem Miraloglu, MD, MS
Functional medicine is a science-based health care approach to assess, prevent and treat complex chronic disease.
![]() Learn More
Learn More
After a brief allergy test, you can begin sublingual immunotherapy (SLIT), or allergy drops under the tongue. No more allergy shots!
![]() Learn More
Learn More
Learn how to prepare for your visit and what to expect at your initial consultation and at your follow-up visits with our office.
![]() Learn More
Learn More