
Your gut microbiome is a pivotal player in your overall metabolic health. One of its significant roles involves influencing the production of glucagon-like peptide-1 (GLP-1), a hormone integral to regulating blood sugar, insulin secretion, appetite, and weight management. In developed countries such as ours, factors including the Western diet, physical inactivity and chronic stress contribute to depletion of the microbes that stimulate GLP-1 production. But all is not lost, keep reading for dietary and lifestyle ways to replenish your microbiome and improve your metabolic health.
Key Microbial Allies
If you are a Carolina Total Wellness patient, your doctor may have asked you to submit a stool test to assess the presence of various specific microbes in your GI tract. Recent research shows that certain gut bacteria are particularly influential in promoting GLP-1 secretion.
Three ways these tiny creatures influence GLP-1 production:
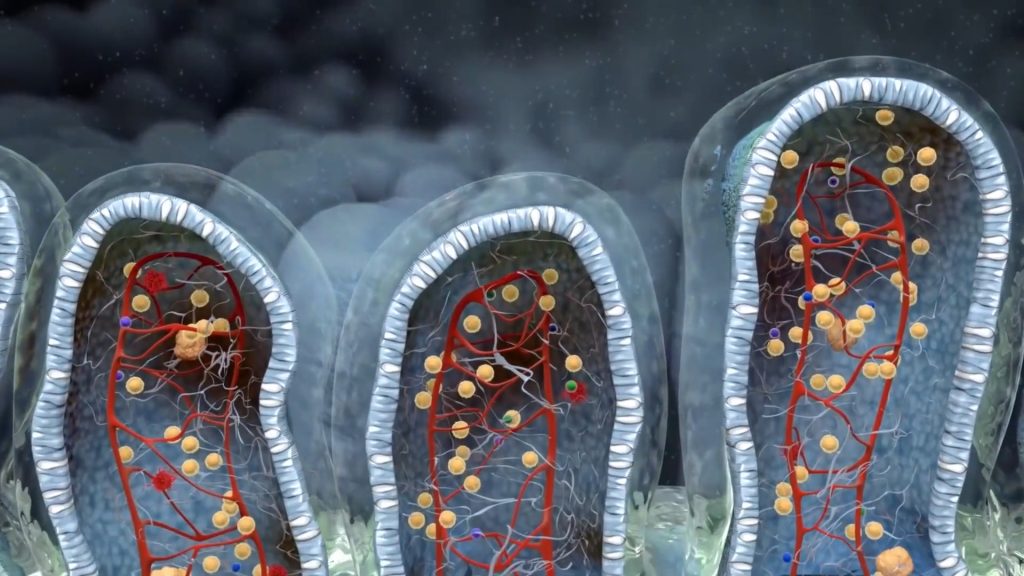
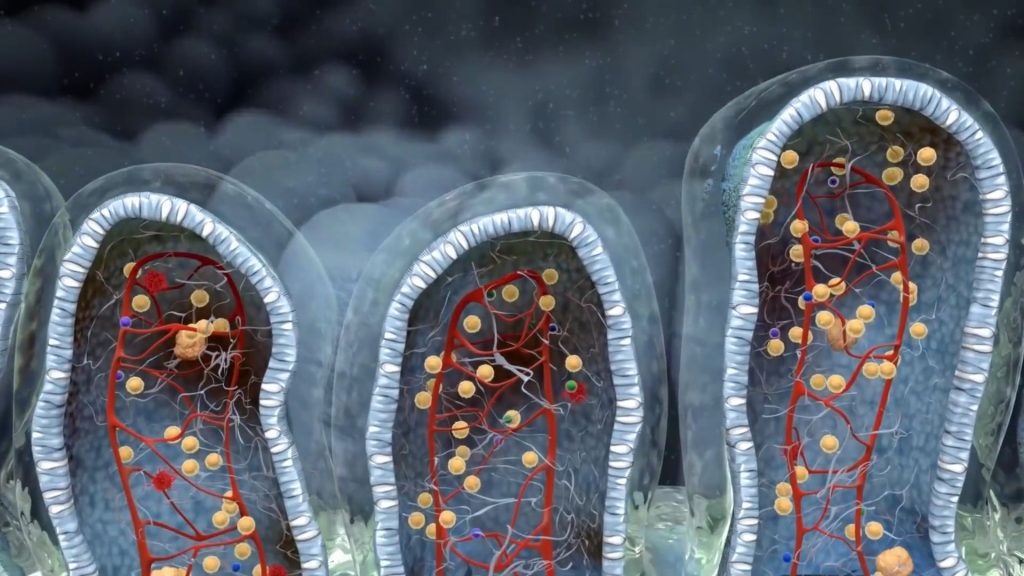
- Fermenting the fiber you eat to produce short-chain fatty acids (SCFAs) and stimulate GLP-1 secretion by intestinal cells.
- Modulating bile acids. Increasing levels to promote GLP-1 secretion.
- Increasing GLP-1 receptor sensitivity, thereby improving the hormone’s ability to regulate glucose metabolism and appetite.
Several keystone bacteria are known ‘influencers’ when it comes to the above processes. Some you may look for on your stool test results include Akkermansia muciniphila, Bacteroides thetaiotaomicron, Faecali- bacterium prausnitzii and Lactobacillus. Akkermansia is especially known for its role in supporting GLP-1 production. Check out last week’s newsletter from our own Dr. Miraloglu to learn more about Akkermansia.
Functional Strategies to Enhance GLP-1 Naturally
To support natural GLP-1 production through microbiome modulation, consider the following approaches:
- Increase Prebiotic Fiber Intake: Foods rich in soluble fiber, such as oats, asparagus, garlic, onions, microgreens, flaxseeds, legumes, and sweet potatoes, serve as prebiotics, nourishing beneficial gut bacteria and promoting short chain fatty acid production (SCFA).
- Incorporate Fermented Foods: Regular consumption of fermented foods like yogurt, kimchi, and sauerkraut introduces beneficial microbes that can support gut health and GLP-1 secretion.
- Supplement Wisely: Specific probiotic supplements can ‘seed’ your microbiome with akkermansia and other beneficial bacteria. Compounds like berberine and N-acetylcysteine (NAC) have been shown to support metabolic health and may enhance GLP-1 levels. Talk to your provider about which supplements may be the best fit for your unique microbiome.
- Diversify Plant Intake: Aim for a variety of plant-based foods to promote microbial diversity, which is linked to robust GLP-1 responses. Can you eat at least 20 different plants each week? Think outside the box, some particularly effective ideas include black or green tea, fruits and vegetables rich in polyphenol antioxidants like apples, beans, berries, cloves, dark chocolate, olives, plums, concord grapes, cranberries and rhubarb.
- Manage Stress: The gut-brain axis is strong. When you experience chronic, unmanaged stress your body diverts resources from the gut to respond to the stress. Regular exercise, a contemplative practice like meditation or yoga and consistent, quality sleep are all beneficial to your microbiome.

The Positive Feedback Loop
Enhancing GLP-1 production not only improves metabolic parameters but also fosters a healthier gut environment. This creates a beneficial cycle where a balanced microbiome supports GLP-1 secretion, and increased GLP-1 further promotes gut health.
By focusing on dietary and lifestyle interventions that support the gut microbiome, we can naturally enhance GLP-1 production, offering a holistic approach to metabolic health. This aligns with the functional medicine principle of addressing root causes rather than merely managing symptoms.
See your functional medicine team at Carolina Total Wellness for tailored recommendations to optimize your microbiome and GLP-1 production.
To schedule an appointment with one of our certified Functional Medicine Physicians, please give us a call. We are excited to partner with you on your journey to optimize your health and wellness through personalized care tailored to your unique needs.
919.999.0831

Your Partner In Health,
Erica Nelson
Health Coach
Carolina Total Wellness
FAQ
WHAT IS GLP- 1 , ANYWAYS?
GLP-1 stands for glucagon-like peptide-1. It is a hormone, produced in the intestine and important for regulating blood sugar, insulin secretion, appetite, and weight management.
WHY ARE SO MANY PEOPLE ON GLP- 1 MEDICATIONS?
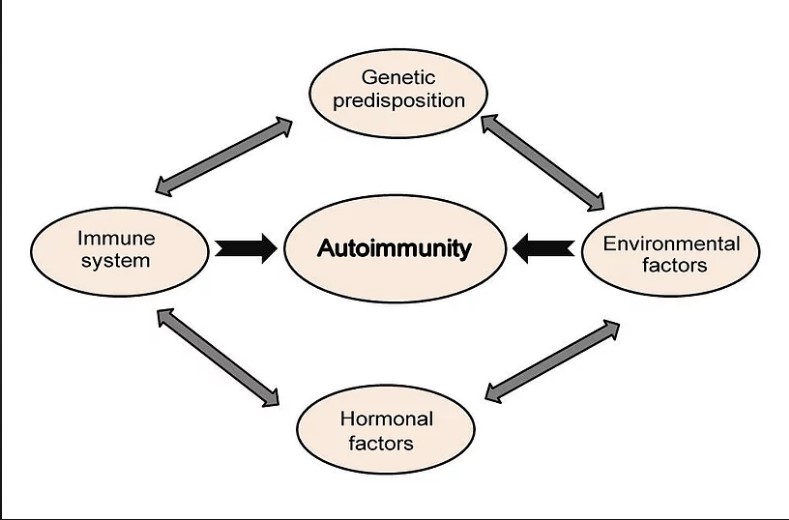
In developed countries such as ours, factors including the Western diet, physical inactivity and chronic stress contribute to depletion of the microbes that stimulate GLP-1 production. People with lower GLP-1 production are more susceptible to a wide variety of maladies including (but not limited to) diabetes, obesity, bowel diseases and metabolic disorders.
HOW CAN I HELP MY BODY MAKE MORE OF MY OWN GLP- 1 ?
Increase prebiotic fiber and fermented food intake, eat at least 20 different plants each week, manage stress and consider supplementing with a probiotic known to support GLP-1 production.