 919-999-0831
919-999-0831

Shane Hemphill, MD
Part II – Low SIgA And How Do We Treat
So your functional medicine provider ordered a Comprehensive Stool Analysis and your SIgA levels are found to be low. What is your next step? The answer is going to vary from person to person, but the ultimate answer is in finding the root cause.
This may include evaluating for and removing a food sensitivity, mold sensitivity, or infection that has over time depleted the immune response.
Once we have eradicated our offending agent we need to look at ways to improve our SIgA levels.
As a general rule the first step is to use an anti-inflammatory diet such as a Mediterranean diet. This is rich in fruits, vegetables, nuts, legumes, olive oil, and fish and low in red meat and saturated fats. One can also eliminate fried foods, processed foods, sugary snacks and soda.
More specific treatments Include:
A diet rich in Polyphenols such as cacao, green tea, and grapeseed extract which have shown to increase SIgA levels.
Saccharomyces Boulardii – This probiotic yeast has been shown to raise SIgA levels while also being very effective against Clostridium Difficile and Candida Overgrowth.
Colostrum – an Immunoglobulin secreted in the early stages of breast-feeding. This has shown to stimulate SIgA levels.
Beta Glucans – This is a type of soluble fiber found naturally in a variety of food sources including oats, barley, rye, rice and mushrooms like Reishi and Shiitaki.
Bone Broth – This is made by simmering the bones and the connective tissue of animals. This forms a stock for making soups, sauces and gravies. Depending on which part you use it contains vitamins, minerals as well as collagen and other amino acids that increase SIgA levels.
Fat Soluble Vitamins – Vitamin A is needed for the transport of SIgA over the mucosal lining. It is suggested that Vitamin A is also involved in the synthesis of other immunoglobulins and has an important influence on our humoral immune system.
Stress Management – Last but not least, Cortisol is the main stress hormone that can decrease SIgA levels. We need to look over your current stressors or perceived levels of stress and then work to reduce them. This can be done through aerobic exercise, yoga, breathing techniques, meditation as well face to face conversations with your friends, family or therapist.
Our functional medicine physicians can help you understand the root cause of low SIgA and design a treatment plan specifically for you, please call our office at 919-999-0831 to get scheduled.
Your Partner in Health!
Shane Hemphill, MD

Clarissa Kussin, ND, FMCHC, ERYT-500

New Year’s is the time when everyone is looking toward the year ahead and all that they want to achieve. While people make resolutions with the best of intentions, few follow through and achieve their goals. This is where health coaching comes in handy.
Health coaches help support clients as they work toward making sustainable lifestyle changes. They are passionate about helping others live happier and healthier lives. This includes helping them stick to New Year’s resolutions. Whether you want to reduce stress, eat better, or move more, health coaches can guide the way.
The Power of Personalized Guidance:
A health coach is your dedicated partner on your wellness journey, offering personalized guidance that goes beyond generic advice. They work with you to create a tailored plan based on your unique needs, preferences, and health goals.
Medical Benefits of Having a Health Coach:
How to Get Started:
If you’re ready to experience the transformative benefits of health coaching, reach out to us today! Our team of experienced health coaches is here to guide you on your journey to optimal health. Call 919.999.0831 to get scheduled.
Remember, investing in your health is an investment in a brighter and more fulfilling future. To your health and happiness!
References:
Wing, R. R., et al. (2018). Intensive lifestyle intervention in type 2 diabetes. New England Journal of Medicine.
Ockene, I. S., et al. (2007). The role of counseling in the promotion of healthy behaviors in adults. JAMA.
Huffman, J. C., et al. (2018). The role of stress and psychosocial interventions in cancer. Current Psychiatry Reports
Warburton, D. E. R., et al. (2006). Health benefits of physical activity: the evidence. Canadian Medical Association Journal
Your Partner In Health,
Clarissa A. Kussin, ND, FMCHC, ERYT-500

| They say that any system is only as strong as its weakest link. It turns out, our digestive and immune systems are only as strong as their weakest leak. Imagine your gut as the body’s security guard. The tight junctions between the cells of your intestines decide who gets in and who doesn’t. But what happens when the gut becomes too permissive and allows unwanted guests through? That’s where “leaky gut” comes into play. Leaky gut, or intestinal permeability, is a condition where the lining of the intestines becomes more porous than it should be. Instead of acting like a strict bouncer to the coolest club in town, the tissue starts allowing substances that shouldn’t enter your bloodstream. This includes undigested food particles, bacteria, and toxins. When the gut barrier is compromised and unwanted intruders enter the bloodstream, your immune system, which usually only targets harmful invaders, can get confused and launch a response against your body’s own tissues instead. It’s like friendly fire within your body! According to the NIH (National Institutes of Health) around 23.5 million (7%) Americans suffer from an autoimmune condition. And 75% of those affected are women. Hashimoto’s thyroid disease, ulcerative colitis, rheumatoid arthritis, psoriasis, vitiligo and multiple sclerosis are some of the more than 80 known autoimmune diseases commonly seen at Carolina Total Wellness. Three Steps to Preventing or Reversing Autoimmune Disease: Not every autoimmune disease is curable or reversible but there are some proven steps you can take to reduce the effects on your health. 1. Manage Your Stress Stress isn’t just in your mind; it affects your gut, too. When we are facing a perceived physical or emotional threat, our bodies are wired to respond by directing resources to your vital organs and away from your digestive and reproductive functions. When you don’t have sufficient digestive enzymes and gastric acid to break foods down, they may be more irritating to your gut lining and/or penetrate the lining as larger particles than your blood stream knows how to handle. It’s not always possible to avoid stress but you can practice strategies to help you minimize the effects. Get 8 consistent hours of sleep each night. Practice saying ‘no’ – it is a full sentence. Go outside and take a walk – without devices. Laugh with a good friend. 2. Eat Gut-Healing Foods Eating a balanced diet is crucial for maintaining gut health. A diet rich in fiber, fruits, and vegetables promotes a diverse gut microbiome and a healthier gut lining. Use the rainbow as a template to guide your shopping list and eat foodsof every color several times per week. Probiotics, found in foods like yogurt, sauerkraut and kimchi help eliminate toxins and aid the digestion of nutrients from the foods you eat. Eat fermented foods several times each week to strengthen the lining of your digestive tract. Bone broth has proteins and gelatin to soothe the inner lining of the gut. Sip on some bone broth instead of coffee in the morning if you’re trying to kick the caffeine habit. 3. Fasting Fridays Once a week, skip breakfast (and the coffee/creamer.) An occasional, extended break from the hard work of digestion, also known as intermittent fasting, lets your gut clean out old debris and calms the immune system. You may discover improved mental clarity and energy, too. In fact, you may like it so much that you decide to skip breakfast two or three days a week. Healing the Gut. If you suspect you have a leaky gut or an autoimmune disease, consult afunctional medicine practitioner. They can recommend personalized approaches like dietary changes, supplementation, and lifestyle modifications to heal your gut and reduce inflammation. Autoimmunity and leaky gut are two puzzle pieces that fit together more than we once thought. Maintaining a healthy gut through a balanced diet, managing stress, and seeking professional guidance when needed can be your key to preventing or managing autoimmune diseases. Remember, the journey to optimal health is unique for everyone. Keep exploring, learning, and making choices that support your well-being. Your Partner In Health, Erica Nelson, MSPH, NBC-HWC |
 |
Katie Depre LAc, LMBT, FABORM, NCCAOM
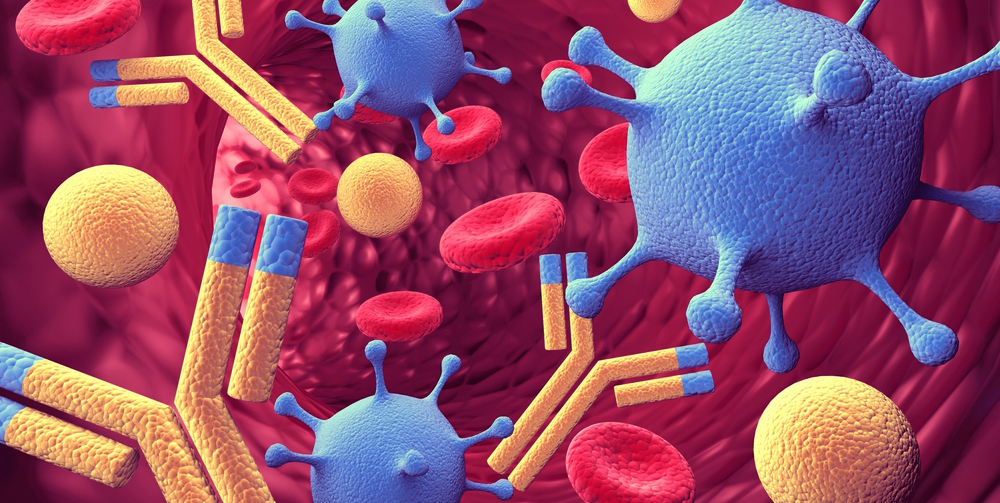
Though often described as traditional or ancient medicine, research has proven that Acupuncture has its place alongside modern medical practices. Hair-thin needles are placed in precise and therapeutic point locations along meridians. Meridians have been shown to mirror the fascial network of the body. Fascia surrounds all of the organs, muscles, bones, and nerve fibers. These points are located alongside nerve endings and blood vessels, thereby directly influencing blood flow and sensory nerves in the area (2,3). Functional brain imaging has shown changes in the brain when these points are needled (1). Since the brain controls the systems of the body (hormones, blood flow, stress responses, organ function, reproduction, etc.), influencing the brain and nervous system with Acupuncture will impact our health. Treatment encourages the body’s own systems of balance, commonly known as homeostasis.
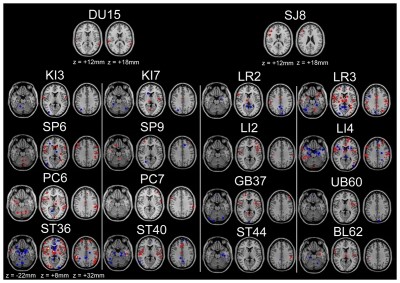
The National Center for Complementary and Integrative Health outlines many of the researched treatable conditions (4); these include: pain management, osteoarthritis, sciatica, fibromyalgia, cancer pain, irritable bowel syndrome, asthma, depression, allergies, infertility, and menopause symptoms. Though more chronic conditions will require a series of treatment for complete resolution, I have personally witnessed immediate relief from insomnia, digestive complaints, anxiety, and pain in my clinic. Especially because it is a non-pharmaceutical approach, many patients search out Acupuncture for treatment to acute and chronic conditions.
As a Fellow of the Acupuncture and Traditional Chinese Medicine Board of Reproductive Medicine, FABORM, I treat many patients with their fertility goals. By regulating the menses, we can prepare the body for pregnancy. Fertility work is best done weekly for three months prior to conception, as it takes three months for the egg to develop in the ovaries. During times of sympathetic stress (the flight or fight response), blood is shunted away from the ovaries and uterus. This can negatively impact egg quality and the thickness of the uterine lining. By encouraging blood flow to these reproductive organs, switching the nervous system into a parasympathetic state (rest, digest, and repair), and regulating the Hypothalamic-Pituitary-Ovarian Axis, we set the body up for success.
For patients undergoing IVF, the Paulus Protocol is utilized. This is a series of points done before and after an embryo transfer. “Clinical pregnancies were documented in 34 of 80 patients (42.5%) in the acupuncture group, whereas the pregnancy rate was only 26.3% (21 out of 80 patients) in the control group (5).”
Please reach out today if you have specific questions on how Acupuncture can help you realize your health goals!
Warmly,
Katie Depre LAc, LMBT, FABORM, NCCAOM
(919) 808-2638
Richard A. Laviano, DC, ND, FSBCT(c)
 |
My doctor has recommended applied kinesiology to rebalance my vagus nerve. Sounds like voodoo to me…. What exactly is applied kinesiology? The importance of the vagus nerve for so many of our bodily function has been proven again and again in multiple medical studies. The vagus nerve runs from your brainstem down to your intestinal tract and is the ringmaster of your autonomic nervous system, all things “rest and digest”. When the vagus nerve is out of balance, it has the potential to create widespread dysfunction from intestinal motility (think small intestinal bacterial overgrowth) to quick “fight or flight” reactivity, anxiety, and even panic attacks. A simple PubMed search of vagus nerve pops up34,789 results! We at CTW have come to rely on the finely tuned skills of practitioners expert in using modalities to rebalance the vagus. One of the most powerful, only in very experienced hands, is applied kinesiology (AK). Dr Rick Laviano of Falls Chiropractic and Injury in Raleigh explains below the role of AK. Applied Kinesiology (AK) is a neurological rehabilitation therapy. At the International College of Applied Kinesiology in 2005 (1) Dr. Walter Schmitt eloquently presented a model that thoroughly explains it. He explains AK as an assessment and therapy that positively affects neurological function. We quote it here and explain it more simply below. AK is a series of sensory receptor based diagnostic challenges followed by monitoring of manual muscle testing outcomes. All AK techniques are about creating sensory receptor stimulation that results in a net effect of excitation and inhibition leading to more optimal neurological function. These positive changes can be observed through somatic windows by changes toward normal in muscle facilitation and inhibition(muscle balance, range of motion, deep tendon reflexes) and through various autonomic windows that can also be monitored (pupil light response, blood pressure, heart rate, etc.) (pg. 1) AK uses muscle tests as well as other neurological tests to assess the state of your nervous system. When there is poor neurological function discovered, the doctor tries his or her best to find the neurological therapy that will improve it. For example, the brainstem (area of the brain just above your neck), controls most of the things in your abdominal cavity subconsciously like your heartrate, blood pressure, gut motility, gut valves, and liver detox. We can see how healthy the brainstem is by looking at reflexes that live there, like how fast your pupils react to a shining light, or how your jaw moves, or how your balance is, or how your blood pressure compares from one side to another (2,4). A physician trained in AK will use these nerdy tools to pinpoint what part of the nervous system may be dormant or over-excited. Then they will wake it up or calm it down through a targeted therapy such as rubbing, tapping, stretching, manipulation, eye movements, muscle/fascial work etc. AK specialists can be considered your body electricians! The ultimate goal is to improve function in the nervous system to thus improve total body health and wellness. Since the nervous system controls every function in our bodies, there have been many types of cases Applied Kinesiologists have seen over the years. Cases that are often seen include gut/microbiome issues. It is important that these patients understand that the gut microbiome is STRONGLY influenced by the state of their gut nervous system. Improving the integrity of the nervous system in these patients can greatly improve their quality of life. Another point worth mentioning regarding gut issues includes the trigeminal nerves. The largest cranial nerve in our brain is the trigeminal nerve. This nerve coordinates information regarding the teeth, jaw, head, and even your posture (3)!This nerve integrates (strongly connects) with the vestibular, ocular, and cerebellar reflexes that affect the health of the brainstem, even the health of the vagus nerve. By keeping the trigeminal nerve and its connections in the brainstem healthy, vagal tone is optimal! In treating gut problems, the priority is making sure that trigeminal, head, eyes, and balance organs are in tune with one another for the health of the autonomic nervous system including the vagus nerve and ultimately the gut. References: 1. Schmitt, Walter H., The Neurological Rationale for a Comprehensive Clinical Protocol Using Applied Kinesiology Techniques. Proceedings of the I.C.A.K. – U.S.A. Annual Meeting, Volume 1,2005-2006. p. 157-191. 2. Monaco, A., Cattaneo, R., Mesin, L., Ciarrocchi,I., Sgolastra, F., & Pietropaoli, D. (2012). Dysregulation of the autonomous nervous system in patients with temporomandibular disorder: a pupillometric study. 3. Cuccia, A., & Caradonna, C. (2009). The relationship between the stomatognathic system and body posture. Clinics, 64(1),61-66. 4. Applied Kinesiology Synopsis: David S. Walther. 1988. Your Partners In Health, Richard A. Laviano, DC, ND, FSBCT(c) and Ana Dávila, DC Falls Chiropractic and Injury, Raleigh NC Frances T Meredith, MD Carolina Total Wellness |
 |

Are you ready for a delightful and soothing beverage that combines the elegance of roses with the goodness of green tea? Introducing Rose-Infused Green Tea, a recipe that nourishes both your senses and your well-being!
Why Rose-Infused Green Tea?
🍵 Green Tea Goodness: Green tea is packed with antioxidants and boasts numerous health benefits. From boosting metabolism to supporting heart health, green tea is a fantastic addition to your daily routine.
🌹 Rose Essence: Roses not only add a delicate floral aroma but also offer their own set of benefits. Rose petals contain antioxidants, vitamins, and minerals that promote skin health, aid digestion, and even have mood-enhancing properties.
Recipe for Rose-Infused Green Tea:
Ingredients:
Instructions:
Benefits of Rose-Infused Green Tea:
1️⃣ Antioxidant Power: Both green tea and rose petals are rich in antioxidants that help combat free radicals, protect cells from damage, and support overall well-being.
2️⃣ Skin Glow: The combination of green tea and rose can promote healthy skin. Antioxidants in green tea and the anti-inflammatory properties of rose petals contribute to a radiant complexion.
3️⃣ Mood Booster: The aroma of roses has been known to uplift the spirit and reduce stress levels. Sipping on Rose-Infused Green Tea can bring about a sense of tranquility and relaxation.
4️⃣ Digestive Aid: Green tea is gentle on the stomach and can support healthy digestion. Combined with the soothing properties of rose petals, it can help alleviate digestive discomfort.
Treat Yourself to a Cup of Bliss… Indulge in the delicate flavors and therapeutic benefits of Rose-Infused Green Tea. This calming and revitalizing beverage is perfect for moments of self-care, relaxation, or whenever you need a little pick-me-up.
Your Partner In Health,
Clarissa A. Kussin, ND, FMCHC, ERYT-500
Sara Yadlowsky, FMHC
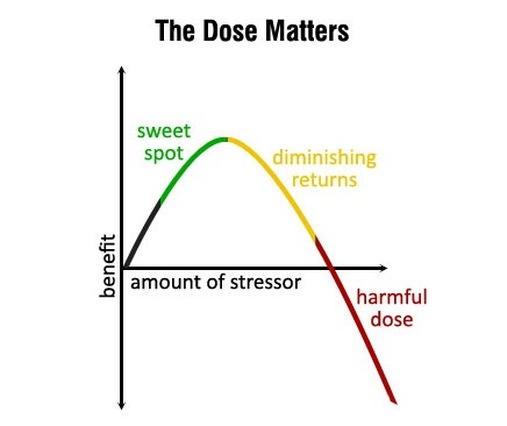
What doesn’t kill you makes you stronger. We’ve all heard the saying before. Science has revealed it is surprisingly accurate when it comes to our health and longevity.
Hormesis is the idea that short, intermittent bursts of certain stressors can start a cascade of cellular processes that slow aging, improve overall health and make you more resilient, both physically and mentally. It is a hot topic in longevity research right now.
We all know that chronic stress caused by relationship issues, financial problems and working too many hours is detrimental to our health. However, hormetic stressors are controlled and acute, triggering healthy adaptive responses.
What does all this mean in real life? Hormesis is the common thread found in some popular health and fitness trends such as HIIT (high intensity interval training), cold exposure, heat therapy and intermittent fasting. Prolonged doses of these behaviors are not healthy or sustainable. For example, if you spend too much time in a sauna you will become dehydrated. But, in short bursts, the bodily stress caused by these practices are enough to bring about health benefits such as reducing inflammation, supporting elimination of toxins, repairing DNA, combatting oxidative stress, repairing cellular damage and reducing risk of cancer.
Here are three ways to strategically stress your body and reap the rewards:
Be aware that adding stress (even the good type!) to our lives can backfire if done at the wrong time. When life is already very stressful, it is best to wait until a better time when you are more relaxed to try out these new practices.
Your Partner In Health,
Sara Yadlowsky, FMHC
Functional medicine is a science-based health care approach to assess, prevent and treat complex chronic disease.
![]() Learn More
Learn More
After a brief allergy test, you can begin sublingual immunotherapy (SLIT), or allergy drops under the tongue. No more allergy shots!
![]() Learn More
Learn More
Learn how to prepare for your visit and what to expect at your initial consultation and at your follow-up visits with our office.
![]() Learn More
Learn More