Erica Nelson, MSPH, NBC-HWC
Practical Strategies for Managing Anxiety and Improving Digestion
Who’s the Boss?
They say the mind is a wonderful servant but a terrible master. Are you in charge of your mind and body? Or do you feel like you are at the mercy of your thoughts and feelings (physical and emotional)? This article shares cost-free and drug-free practical strategies to take back control of your physical and emotional feelings and make your mind your servant.
Your nervous system is complicated but you do not need to know all of the details to have a significant impact on its function. In this article you will find a very simple description of how one specific nerve, the Vagus, connects your physical and emotional feelings. You will also learn practical things you can do to reduce anxiety, improve digestion and overall wellbeing.
A (Very) Brief Neuroanatomy Lesson
Starting from the top, the brain branches out from your skull through 12 cranial nerves (and their branches) known as the peripheral nervous system.

Starting from the ‘bottom’ the gastrointestinal ‘mind’ is called the enteric nervous system (ENS.) The ENS has more nerve cells than the rest of the entire nervous system combined (more than 100 million!) and is capable of functioning independently of the rest of the nervous system.
The Vagus nerve is one of the 12 cranial nerves. It connects your brain to your digestive system and vice versa. It sends and receives both motor (movement) and sensory (feeling) signals. Beyond the digestive system, it touches nearly every major organ and plays a role in heart rate, respiration, facial expression, inflammation, sweating, reproduction and more.
Photo courtesy:
www.drarielleschwartz.com

The word ‘Vagus’ comes from the Latin for ‘wander’ but, as Tolkien wisely said, ‘Not all who wander are lost.’ This nerve, and its branches serve as the information super highway in your body and provide the early warning system for threats, internal and external.
Most of these functions are reflexes that happen without you thinking about them to keep you alive. Can you imagine if you had to decide to shunt blood supply from your stomach to your heart and lungs to run from danger? But sometimes the reflexes are not actually helpful in the moment and we are left feeling like our stomachs have minds of their own – because they kind of do. But when we know what the reflexes respond to, we can take steps to trigger a more desirable response.
Toning the Vagus for Stress Resilience
Have you ever felt your mouth go bone dry just as you are about to begin a presentation or performance? Or worse, maybe you feel like you are going to throw up? Or need to go to the bathroom RIGHT NOW. This is your reflexive response to stop bodily secretions and smooth muscle contractions in your GI tract so you can spend your resources elsewhere.
When you perceive a threat, your brain and body make preparations to respond and additional resources – oxygen, fluids, etc. – are diverted from digestion and reproduction until you are physically and psychologically safe again. Your heart rate, blood pressure and breathing increase, your pupils dilate, your mouth may go dry, your muscles may begin to tremble all of these are signs of activation of your sympathetic nervous system.
It is the job of the parasympathetic nervous system, including the Vagus nerve, to restore resources to ‘rest and digest’ once the threat (perceived or real) is passed. Depending on the duration and intensity of the threat, it may take 20 minutes or 20 years to return to a healthy resting state. When left unattended, chronic stress or PTSD can have long-term effects on your physical, cognitive and emotional health.
Techniques to Build ‘Stress Resillience’ and Facilitate the Job of the Vagus Nerve
Daily Habits to Support Stress Resilience:
- Cat/Cow stretching with a Lion’s Roar
This exercise lengthens and contracts the Vagus nerve to activate it. Get on your hands and knees on the floor. Begin with a neutral spine and then press down through your hands and knees to arch your back upwards like a cat. Inhale while doing this. Then drop your belly down towards the floor and lift your breastbone forward and up. Exhale loudly while you do this, sticking your tongue out and even roaring like a lion.
- Laugh
Laughter really is one of the best medicines. Real laughter is best but even fake laughter will engage the Vagus nerve through contraction of the diaphragm.
- Hugs
A warm embrace, ideally 20 seconds or longer, will stimulate the part of the Vagus nerve that runs down your back and can trigger the release of a hormone called oxytocin, known as the feel-good hormone.
- Singing, humming, chanting, gargling
The Vagus nerve is connected to your vocal cords and the muscles at the back of your throat. All of these activities activate the muscles around the nerve and can stimulate it. Choose one or more and find time for it each day.
In-the-Moment Strategies to Get Back to Rest and Digest:
- 4-7-8 breathing
Place the tip of your tongue against the ridge of tissue just behind your upper front teeth, and keep it there through the entire exercise. Exhale completely through your mouth, making a whoosh sound. Close your mouth and inhale quietly through your nose to a mental count of four. Hold your breath for a count of seven. Exhale completely through your mouth, making a whoosh sound to a count of eight. This is one breath. Now inhale again and repeat the cycle three more times for a total of four breaths.
- Go outside for a walk
This works for a couple of reasons. First, when you are walking, your eyes naturally move side-to-side and trigger a response in your brain that distracts it from threat. Second, you are using up some of the ‘energy hormones’ that were dumped into your system to respond to the threat and may be making you feel ‘jittery.’
- Self-massage
Stroke your neck from your ear to your clavicle 10 times on each side. Again, your Vagus nerve is connected to these muscles. Moderately intense massage to the area will stimulate the nerve and help to restore a resting state.
You do not have to be at the beck and call of your body’s reflexes. Choose one or two of the strategies above and integrate them into your day to improve your ability to respond the way you want to – instead of simply reacting – the next time you are faced with a stressful situation.
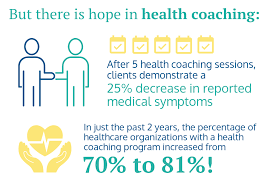
Call our office and schedule an appointment with one of our health coaches to learn more healthy strategies to reduce and respond to physical, emotional and cognitive stress.
Your Partner in Health!
Erica Nelson, MSPH, NBC-HWC