If you have been researching how to improve your health, you may have heard of leaky gut, also known as intestinal permeability. If that conjures an unpleasant image of your gut contents leaking into the rest of your body — that’s not too far off the mark.
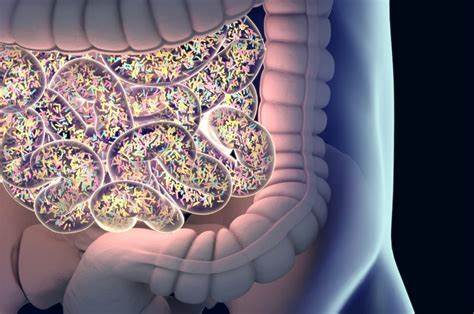
Leaky gut happens when contents from the small intestine spill into the sterile bloodstream through a damaged and “leaky” gut wall. This contamination of the bloodstream by not only partially digested foods but also bacteria, yeast, and other pathogens begins to create a foundation for chronic inflammatory and autoimmune health disorders.
Symptoms and disorders linked to leaky gut include fatigue, depression, brain fog, skin problems, joint pain, chronic pain, autoimmune disease, puffiness, anxiety, poor memory, asthma, food allergies and sensitivities, seasonal allergies, fungal infections, migraines, arthritis, PMS, and many more. Basically, your genetic predispositions will determine how leaky gut manifests for you.
Leaky gut is referred to as intestinal permeability in the scientific research. It means inflammation has caused the inner lining of the small intestine to become damaged and overly porous. This allows overly large compounds into the small intestine. The immune system recognizes these compounds as hostile invaders that don’t belong in the bloodstream and launches an ongoing attack against them, raising inflammation throughout the body. Also, some of these compounds are very toxic (endotoxins) and take up residence throughout the body, triggering inflammation wherever they go.
At the same time, excess intestinal mucous and inflammation from the damage prevents much smaller nutrients from getting into the bloodstream, which can lead to nutrient deficiencies and poor cellular function.
Leaky gut is increasingly being recognized as a common underlying factor in most inflammatory symptoms and disorders.
Medicine finally recognizes leaky gut
Conventional medicine has long ridiculed leaky gut information and protocols as quack science and alternative medicine folklore, but newer research now establishes it as a legitimate mechanism. In fact, pharmaceutical companies are even working on drugs to address leaky gut.
Research has established links between leaky gut and many chronic disorders. It’s good this long-known information is finally being validated in the dominant medical paradigm as the gut is the largest immune organ, powerfully influencing the rest of the body, as well as the brain.
Current studies link intestinal permeability with inflammatory bowel disorders, gluten sensitivity, celiac disease, Crohn’s disease, type 1 diabetes, depression, psoriasis, and other chronic and autoimmune conditions. Given what we know about the connection between gut health and immunity, it’s vital to include a gut repair protocol in overall treatment of inflammatory and autoimmune disorders.
How to mend leaky gut
Sometimes, repairing leaky gut can be as simple as removing inflammatory foods from your diet. Other times it’s more complicated. Most importantly, you need to know why you have leaky gut. Either way, however, your diet is foundational.
Many cases of leaky gut stem from a standard US diet of processed foods and excess sugars. Food intolerances also contribute significantly, especially a gluten intolerance. A leaky gut diet, also known as an autoimmune diet, has helped many people repair intestinal permeability. Keeping blood sugar balanced is also vital. If blood sugar that gets too low or too high, this promotes leaky gut. Stabilizing blood sugar requires eating regularly enough to avoid energy crashes. You also need to prevent high blood sugar by avoiding too many sugars and carbohydrates. Regular exercise is also vital to stabilizing blood sugar and promoting a healthy gut.
Also, failure to eat enough fiber and produce leads to leaky gut by creating a very unhealthy gut microbiome, or gut bacteria. Our intestines (and entire body) depend on a healthy and diverse gut microbiome for proper function. A healthy gut microbiome comes from eating at least 25 grams of fiber a day and a wide and rotating variety of plant foods.
Other common things that lead to leaky gut include antibiotics, NSAIDs such as ibuprofen, excess alcohol, hypothyroidism, and autoimmunity.
A leaky gut protocol can help you improve your health, relieve symptoms, boost energy, make you happier, and clear your brain fog. Ask my office for advice on improving your well being through a leaky gut diet and protocol.