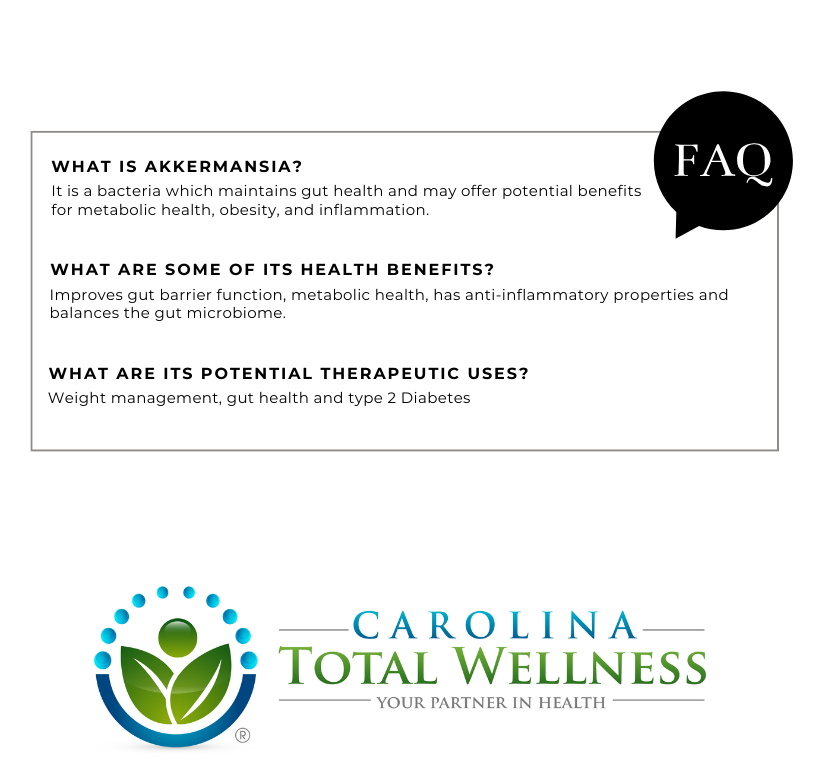
Akkermansia is a fascinating bacterium that plays a key role in maintaining gut health and may offer potential benefits for metabolic health, obesity, and inflammation. Research into its therapeutic applications continues to evolve, and it could be a key player in future microbiome-based treatments.
WHAT ARE SOME OF THE KEY POINTS OF AKKERMANSIA?
1. Role in the Gut:
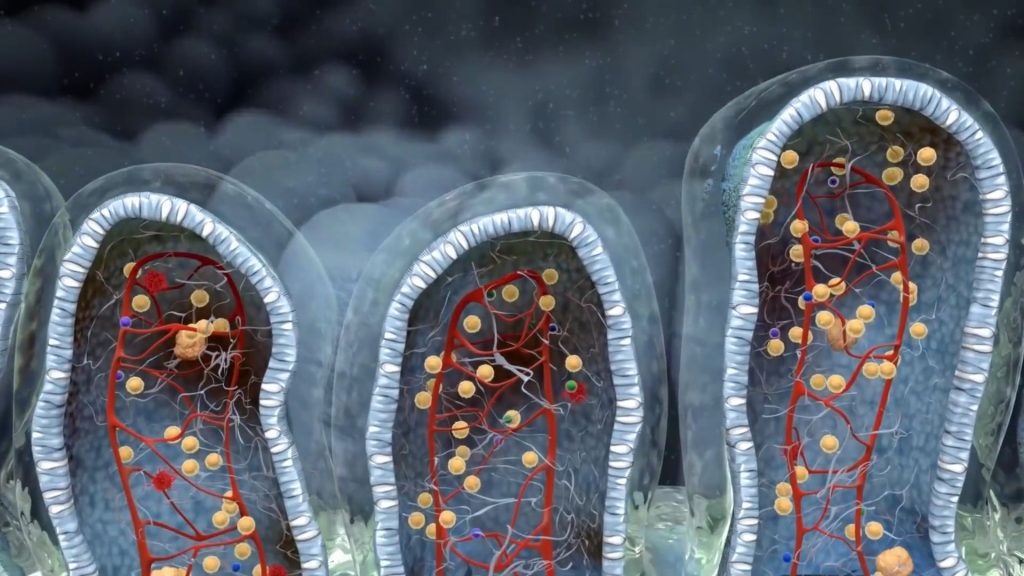
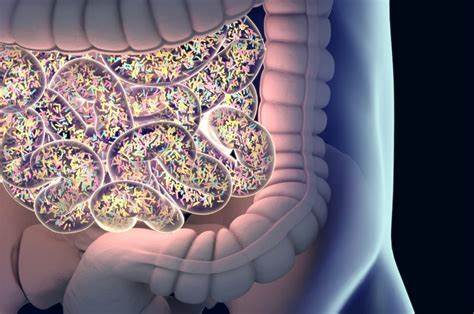
Akkermansia muciniphila is a type of mucin-degrading bacterium, meaning it breaks down mucin, which is a major component of the mucus lining the intestines. By doing this, Akkermansia helps maintain the integrity of the gut lining and may play a role in gut health.
2. Health Benefits:
Research suggests that Akkermansia may have several beneficial effects on health, including:
- Improving Gut Barrier Function: It helps in maintaining a healthy mucus layer in the intestines, which acts as a barrier to harmful pathogens and supports gut health.
- Metabolic Health: Studies have shown that higher levels of Akkermansia muciniphila are linked to improved metabolic health. It may help with weight management and insulin sensitivity, potentially reducing the risk of obesity and type 2 diabetes.
- Anti-inflammatory Properties: Akkermansia may help reduce inflammation, which is associated with many chronic diseases, such as cardiovascular disease, inflammatory bowel disease (IBD), and others.
- Gut Microbiome Balance: Akkermansia is considered a “beneficial” bacterium, and higher levels of it may be associated with a more diverse and healthy gut microbiome, which is crucial for overall health.
3. Factors Affecting Its Levels:
The levels of Akkermansia muciniphila in the gut can be influenced by various factors, including diet, lifestyle, and overall gut health. For example:
- Dietary Fiber: A diet rich in dietary fiber, especially from fruits, vegetables, and whole grains, can promote the growth of Akkermansia.
- Prebiotics and Probiotics: Certain prebiotic fibers and probiotics might help increase the abundance of Akkermansia in the gut.
- Obesity and Metabolic Disorders: Lower levels of Akkermansia have been found in individuals with obesity, type 2 diabetes, and metabolic syndrome.
4. Potential Therapeutic Uses:
Researchers are investigating the use of Akkermansia muciniphila in therapeutic applications, including as a probiotic. The potential benefits include:
- Weight Management: Studies have suggested that Akkermansia supplementation may help with weight loss and metabolic health, although more research is needed.
- Gut Health: Akkermansia supplementation may help restore balance to the gut microbiome and improve conditions like irritable bowel syndrome (IBS) or IBD.
- Type 2 Diabetes: There is ongoing research into how Akkermansia may help improve insulin sensitivity and glucose metabolism.
5. Research and Future Directions:
While much of the current research into Akkermansia is still in the experimental stages, its potential for improving gut health and metabolic conditions is promising. However, more clinical trials are necessary to fully understand its therapeutic applications and optimal usage.

At Carolina Total Wellness, we evaluate the levels of Akkermansia through a stool test and treat you accordingly on whether this probiotic would benefit you.
Come see us about what the hype is all about!
To schedule an appointment with one of our certified Functional Medicine Physicians, please give us a call. We are excited to partner with you on your journey to optimize your health and wellness through personalized care tailored to your unique needs.
919.999.0831