Follow Carolina Total Wellness on Social Media!
 919-999-0831
919-999-0831
Follow Carolina Total Wellness on Social Media!


Shane Hemphill, MD
Part II – Low SIgA And How Do We Treat
So your functional medicine provider ordered a Comprehensive Stool Analysis and your SIgA levels are found to be low. What is your next step? The answer is going to vary from person to person, but the ultimate answer is in finding the root cause.
This may include evaluating for and removing a food sensitivity, mold sensitivity, or infection that has over time depleted the immune response.
Once we have eradicated our offending agent we need to look at ways to improve our SIgA levels.
As a general rule the first step is to use an anti-inflammatory diet such as a Mediterranean diet. This is rich in fruits, vegetables, nuts, legumes, olive oil, and fish and low in red meat and saturated fats. One can also eliminate fried foods, processed foods, sugary snacks and soda.
More specific treatments Include:
A diet rich in Polyphenols such as cacao, green tea, and grapeseed extract which have shown to increase SIgA levels.
Saccharomyces Boulardii – This probiotic yeast has been shown to raise SIgA levels while also being very effective against Clostridium Difficile and Candida Overgrowth.
Colostrum – an Immunoglobulin secreted in the early stages of breast-feeding. This has shown to stimulate SIgA levels.
Beta Glucans – This is a type of soluble fiber found naturally in a variety of food sources including oats, barley, rye, rice and mushrooms like Reishi and Shiitaki.
Bone Broth – This is made by simmering the bones and the connective tissue of animals. This forms a stock for making soups, sauces and gravies. Depending on which part you use it contains vitamins, minerals as well as collagen and other amino acids that increase SIgA levels.
Fat Soluble Vitamins – Vitamin A is needed for the transport of SIgA over the mucosal lining. It is suggested that Vitamin A is also involved in the synthesis of other immunoglobulins and has an important influence on our humoral immune system.
Stress Management – Last but not least, Cortisol is the main stress hormone that can decrease SIgA levels. We need to look over your current stressors or perceived levels of stress and then work to reduce them. This can be done through aerobic exercise, yoga, breathing techniques, meditation as well face to face conversations with your friends, family or therapist.
Our functional medicine physicians can help you understand the root cause of low SIgA and design a treatment plan specifically for you, please call our office at 919-999-0831 to get scheduled.
Your Partner in Health!
Shane Hemphill, MD

Clarissa A. Kussin, ND, FMCHC, ERYT-500

As we journey through spring, it’s crucial to ensure our homes remain safe havens for our respiratory health. Many common household cleaners contain chemicals that provoke or worsen asthma or COPD symptoms, making cleaning uncomfortable and potentially dangerous. It is also important to consider our indoor air quality by using more eco-friendly products and lowering our risk of asbestos exposure which can be found in some houses, and in the long run, can affect the lungs developing. Today we’re focusing on sourcing lung-friendly household products to support your well-being.
1. Understanding Lung-Safe Products: Choosing the right household products can significantly impact respiratory health. Opting for lung-safe options reduces exposure to volatile organic compounds (VOCs), fragrances, and other irritants. Look for products labeled as “fragrance-free,” “non-toxic,” and “low VOC.”
2. Recommended Brands: We’ve curated a list of reputable brands known for their commitment to lung-safe products:
3. DIY Lung-Safe Alternatives: For those who prefer a hands-on approach, crafting your own cleaners allows full control over ingredients. Simple, lung-safe recipes often include ingredients like baking soda, vinegar, castile soap, and essential oils (for those not sensitive to them). Check out reputable sources like the Environmental Working Group (EWG) for safe DIY recipes.
4. Resources for Lung-Safe Living: Stay informed and empowered with these valuable resources:
Remember, small changes can make a big difference in supporting respiratory wellness and investing in your health is an investment in a brighter and more fulfilling future. Stay safe and breathe easy!
If you’re ready to experience the transformative benefits of health coaching, reach out to us today! Our team of experienced health coaches are here to guide you on your journey to optimal health. Call 919.999.0831 to get scheduled.
To your health and happiness!
Clarissa A. Kussin, ND, FMCHC, ERYT-500

Sara Yadlowsky, FMHC

Aging is inevitable. Irrespective of our efforts to appear youthful or feel younger, aging will catch up with us eventually. However, vitality is the key to aging gracefully.
Vitality embodies an energy of involvement, appreciation, and liveliness. It represents a harmonious blend of pleasure, purpose, and significance. When we are full of these feelings, we experience a vibrant, open responsiveness.
An excellent question to ask yourself is: How vibrant am I? Vitality manifests as an ability to openly express profound emotions. It’s evident in hearty laughter, streams of tears, and a willingness to engage fully without concerning oneself with outcomes, approval, or social media “likes.”
The most vibrant individuals:
This level of aliveness represents soulful fitness, which is not tied to appearing younger than our years. Soulful fitness results from a stead fast commitment to and consistent practice of the vitality-enhancing measures mentioned above.
An excellent idea is to meditate daily with the thought that this could be your last day alive, and let this awareness guide you to fully embrace and cherish each day.
Aging can be viewed as a profound opportunity to establish deeper roots and witness more abundant blossoms. We can perceive the beautiful trajectory from innocence (youth) to ambition (productive years) to wisdom (later years)as a magnificent symphony, with each phase a complete and essential component of a breathtaking unity.
Aging is not an error or shortcoming, but an invitation to embrace life more fully.
To schedule a new patient or health coaching appointment, please call our office at 919-999-0831.
Your Partner in Health!
Sara Yadlowsky, FMHC
Didem Miraloglu, MD, MS

| Nitric oxide (NO) is a remarkable molecule that plays a crucial role in various physiological processes within the human body. Discovered in the late 18th century, and its importance has been extensively studied and recognized in the fields of medicine, biology, and biochemistry. In fact in 1998 Nobel Prize in Physiology or Medicine was awarded to Robert Furchgott, LouisIgnarro, and Ferid Murad, for their discoveries of NO as a signal molecule in the vasculature and specifically in the control of blood pressure. NO is a unique signaling molecule that influences numerous cellular pathways, contributing to cardiovascular health, immune function, neurotransmission, and even cellular defense against pathogens. The synthesis of nitric oxide is achieved through the enzymatic action of nitric oxide synthase (NOS) on L-arginine, a semi-essential amino acid found in the body. There are three isoforms of NOS: endothelial NOS(eNOS), neuronal NOS (nNOS), and inducible NOS (iNOS). Each isoform is expressed in specific tissues and cells and responds to different stimuli. eNOSis predominantly present in endothelial cells, contributing to vasodilation and regulating blood flow. nNOS is found in neurons and plays a role in neuro transmission, while iNOS is induced in response to inflammation or immune challenges. The regulation of nitric oxide production is a tightly controlled process. Various factors, including calcium ions, cofactors like tetrahydrobiopterin, and the availability of L-arginine, affect NOS activity. This precise control ensures that NO is produced when needed, preventing excessive generation and potential cellular damage. Nitric oxide is a key player in cardiovascular health. It acts as a vasodilator, relaxing the smooth muscles in blood vessel walls, which leads to increased blood flow and improved oxygen and nutrient delivery to tissues. Dysfunction in the NO pathway is associated with numerous cardiovascular diseases, including hypertension, atherosclerosis, and heart failure. Pharmaceutical agents that enhance NO production or mimic its actions, such as nitroglycerin and sildenafil (Viagra), have become essential treatments for these conditions. The immune system relies on nitric oxide to fight off pathogens and defend against infections. When activated by cytokines and other immune molecules, iNOS produces NO in macrophages and other immune cells. Nitric oxide acts as a potent antimicrobial agent by damaging bacterial DNA, proteins, and lipids. Furthermore, it helps regulate the immune response and plays a role in resolving inflammation after an infection has been controlled. In the nervous system, nitric oxide is a critical neurotransmitter involved in various processes, such as learning and memory, synaptic plasticity, and neuronal communication. It modulates the release of neurotransmitters like dopamine, serotonin, and glutamate, contributing to mood regulation and cognition. Moreover, NO has been linked to neuroprotection by its ability to act as an antioxidant and counteract oxidative stress-induced damage. Neurodegenerative diseases, such as Alzheimer’s and Parkinson’s, involve oxidative stress, and researchers are exploring the potential of NO-based therapies to mitigate neuronal damage. Due to its diverse roles in numerous physiological processes, nitric oxide has garnered significant interest as a potential therapeutic agent. Researchers are exploring its use in various medical applications, including wound healing, erectile dysfunction, and respiratory disorders like pulmonary hypertension. Additionally, NO-based therapies are being investigated in the context of cancer treatment, where NO has shown potential to inhibit tumor growth and sensitize cancer cells to radiation and chemotherapy. Nitric oxide, once regarded merely as an air pollutant, has emerged as a fundamental molecule essential for life and well-being. Its roles in cardiovascular health, immune function, neurotransmission, and neuroprotection highlight its significance in maintaining the body’s delicate balance. As our understanding of this remarkable molecule deepens, we are likely to witness further advancements in medical therapies that harness the potential of nitric oxide for improving human health and well-being. To schedule a new patient appointment, please call our office at 919-999-0831. Your Partner In Health, Didem Miraloglu, MD, MS |
 |
Clarissa A. Kussin, ND, FMCHC, ERYT-500
Did you know that REM (Rapid Eye Movement) sleep is a game-changer for your overall health and well-being? Let’s dive into the incredible benefits of REM sleep and discover some tips to enhance your dreamy slumber!
Benefits of REM Sleep:
Tips to Maximize REM Sleep:
Prioritize your sleep, and watch the positive impact on your overall well-being!
If you’re ready to experience the transformative benefits of health coaching, reach out to us today! Our team of experienced health coaches is here to guide you on your journey to optimal health. Call 919.999.0831 to get scheduled.
Remember, investing in your health is an investment in a brighter and more fulfilling future.
To your health and happiness!
Clarissa A. Kussin, ND, FMCHC, ERYT-500

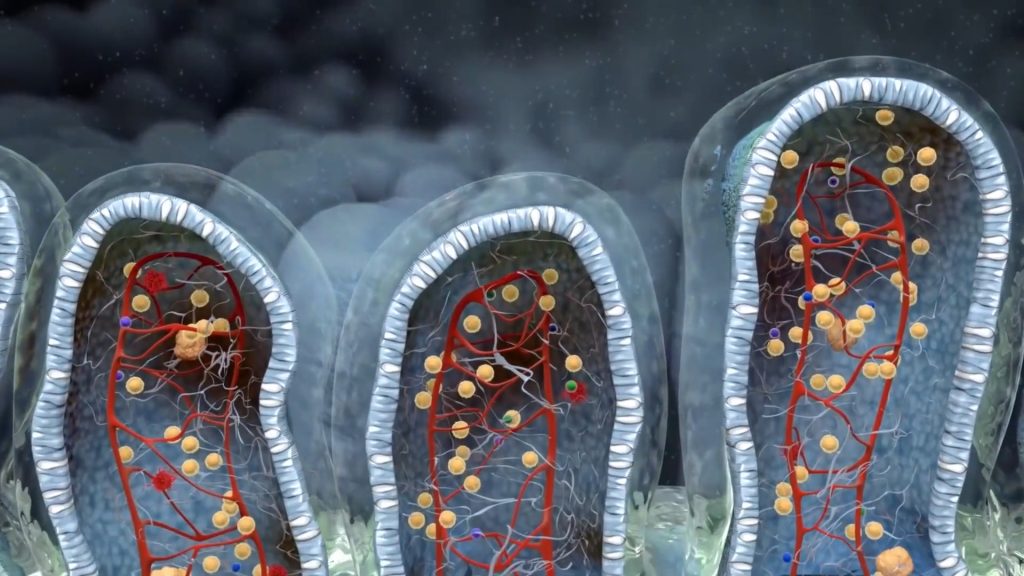
Shane Hemphill, MD
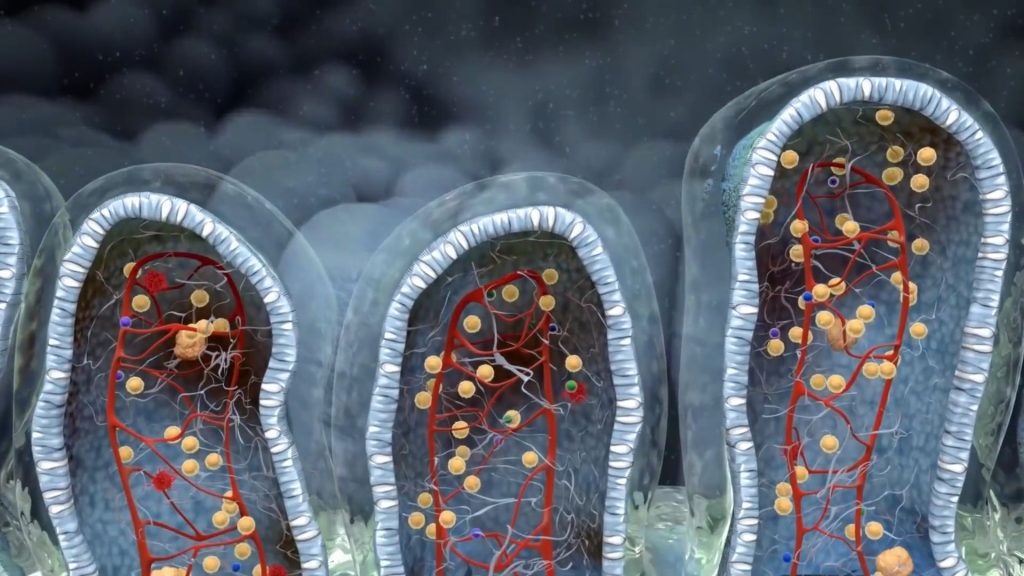
| Say your functional medicine provider ordered a stool test and it showed Low SIgA- what does that mean and how did it develop? The immune system makes T cells and B cells. The B cells produce secretory IgA (SIgA) which acts as a first line of defense against the entry of foreign substances into the body. These foreign substances include many things such as undigested proteins from the foods that we eat, bacteria, viruses, parasites, or even molds. In essence SIgA gives us insight into what is happening at our mucosal surfaces. The body’s mucosal surfaces – located at the eyes, ears, nose, throat, sinuses, gastrointestinal and genitourinary tracts, and skin are all entry points for potential disease-causing pathogens. Our body’s way of protecting these entry points is done with the release of SIgA. B-cells present within the mucosa are activated upon exposure to pathogens and allergens and thus produce SIgA in response. The SIgA then attaches itself to the invading bacteria, virus or other foreign substance, traps it in the mucosal surface and then neutralizes it. So what does it mean if your SIgA is low? If your SIgA is low, this means that you are less able to prevent invaders from getting into your gut mucosal lining. This lining can become inflamed and tight junctions that ordinarily keep toxins and undigested food particles out – break down. This causes havoc as now toxins and undigested substances are able to get access to our blood stream, causing inflammatory and immune reactions that lead to systemic symptoms throughout the body. Patients with low SIgA levels generally have increased risk of food sensitivities, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), intestinal permeability also known as ‘leaky gut’, autoimmunity, and other gastrointestinal infections. What causes low SIgA levels? Chronic infections are commonly associated with low SIgA. Assessing for problematic bugs including H pylori, Candida, Blastocystis Hominis, H. Pylori, Clostridium difficile are essential in this evaluation. Do keep in mind that many of these normally can exist in the bowel at low levels and not cause harm. Some of them only become problematic depending on their level in the body and others do it based on virulence. These can be assessed via a functional stool test. One interesting note is that these ‘infections’ are opportunistic by nature, meaning they also come about when SIgA levels reduce. Therefore it is not uncommon to see development of Candida in SIgA compromised clients. Medications are another cause of low SIgA. Anti-inflammatories, antibiotics and antidepressants are some examples. Studies have even shown an association between low SIgA and people that suffer from depression. Stress is another cause of low SIgA through increased cortisol levels. Stress can be in any form, including mental, emotional or even physical. One study has even demonstrated that persistent negative thoughts about ourselves can lower our own SIgA levels. Lowering stress and introducing stress reduction techniques is vital in maintaining this protector. Finally, poor dietary choices are another contributor to low SIgA. Certain nutrients such as Vitamin D, Vitamin A, Zinc and Glutathione are instrumental in supporting healthy SIgA levels. A good intake of dietary fiber and phytonutrients can also play a role in supporting a healthy gut microbiome. This can lead to the development of beneficial bacteria that promote healthy levels as well. Stay tuned for my next article which will discuss how we treat low SIgA. To schedule a new patient appointment, please call our office at 919-999-0831. Your Partner in Health! Shane Hemphill, MD |
 |
Didem Miraloglu, MD, MS

Za’atar is a Middle Eastern spice blend that typically includes a mix of dried thyme, oregano, marjoram, sumac, sesame seeds, and salt. It’s a staple in Palestinian cuisine and is used in various dishes, such as meats, salads, bread, and dips. While specific health benefits can vary based on individual ingredients and their proportions in the blend, here are some potential health benefits associated with Palestinian za’atar:
1. Rich in Antioxidants: Thyme, oregano, and sumac, commonly found in za’atar, are rich in antioxidants that help fight oxidative stress and reduce the risk of chronic diseases.
2. Anti-inflammatory Properties: Many of the herbs in za’atar, like thyme and oregano, contain compounds that possess anti-inflammatory properties, potentially aiding in reducing inflammation in the body.
3. Digestive Health: Some of the herbs in za’atar, like thyme and oregano, are believed to have digestive benefits, aiding in digestion and potentially soothing digestive issues.
4. Possible Antibacterial and Antifungal Effects: Some studies suggest that certain compounds in thyme and oregano may have antibacterial and antifungal properties, which could help infighting off infections.
5. Improved Cognitive Function: Rosemary, sometimes included in za’atar blends, has been linked to improved cognitive function and memory.
6. Rich in Nutrients: Sesame seeds in za’atar provide healthy fats, protein, and important minerals like calcium, magnesium, and zinc.
It’s incredibly versatile and can be used in various recipes.
Here are a few ideas:
1. Za’atar Hummus:
Blend chickpeas, tahini, garlic, lemon juice, olive oil, and a generous amount of za’atar until smooth. Adjust seasoning to taste. Serve with pita bread or vegetable sticks.
2. Za’atar Roasted Vegetables:
Toss vegetables like cauliflower, carrots, and zucchini in olive oil, sprinkle with za’atar, salt, and pepper. Roast in the oven until golden brown and tender.
3. Za’atar Grilled Chicken:
Marinate chicken breasts or thighs with olive oil, lemon juice, garlic, and za’atar. Grill until fully cooked and serve with a side of yogurt sauce mixed with a bit of za’atar.
4. Za’atar Flatbread:
Mix za’atar with olive oil and spread it over flatbread dough. Bake until golden and crispy. Enjoy it as a side to dips, soups, or salads.
5. Za’atar Salad Dressing:
Whisk together olive oil, lemon juice, a dash of honey, salt, pepper, and za’atar. Drizzle over a mixed green salad or a chickpea salad for added flavor.
6. Za’atar-Crusted Fish:
Mix za’atar with breadcrumbs or almond meal. Coat fish fillets in the mixture and bake or pan-sear until the crust is crispy and the fish is cooked through.
7. Za’atar Focaccia Bread:
Add za’atar to the dough when making focaccia bread. Sprinkle extra on top along with olive oil before baking.
8. Za’atar Popcorn:
Sprinkle popped popcorn with melted butter or olive oil and za’atar for a unique and flavorful snack.
9. Za’atar Potatoes:
Toss potato wedges with olive oil and za’atar. Roast them until crispy on the outside and tender on the inside.
10. Za’atar Yogurt Dip:
Mix za’atar into Greek yogurt along with a little garlic powder, lemon juice, salt, and pepper. Serve as a dip for veggies, pita chips, or crackers.
Feel free to adjust the quantities of za’atar based on your taste preferences. It’s a versatile spice blend that can add a unique and delicious flavor to various dishes!
It’s essential to note that while these herbs and spices offer potential health benefits, they are typically consumed in small amounts as part of a larger diet. The overall health effects will also depend on an individual’s diet and lifestyle. Additionally, the specific composition of za’atar can vary, so the health benefits might differ accordingly.
As with any food or spice, moderation is key. Incorporating za’atar into a well-balanced diet can be a flavorful way to potentially enjoy some health benefits, but it should be part of an overall healthy lifestyle. If you have specific health concerns or conditions, it’s advisable to consult with a healthcare professional for personalized advice.
Your Partner In Health,
Didem Miraloglu, MD, MS

Functional medicine is a science-based health care approach to assess, prevent and treat complex chronic disease.
![]() Learn More
Learn More
After a brief allergy test, you can begin sublingual immunotherapy (SLIT), or allergy drops under the tongue. No more allergy shots!
![]() Learn More
Learn More
Learn how to prepare for your visit and what to expect at your initial consultation and at your follow-up visits with our office.
![]() Learn More
Learn More