 919-999-0831
919-999-0831
 |
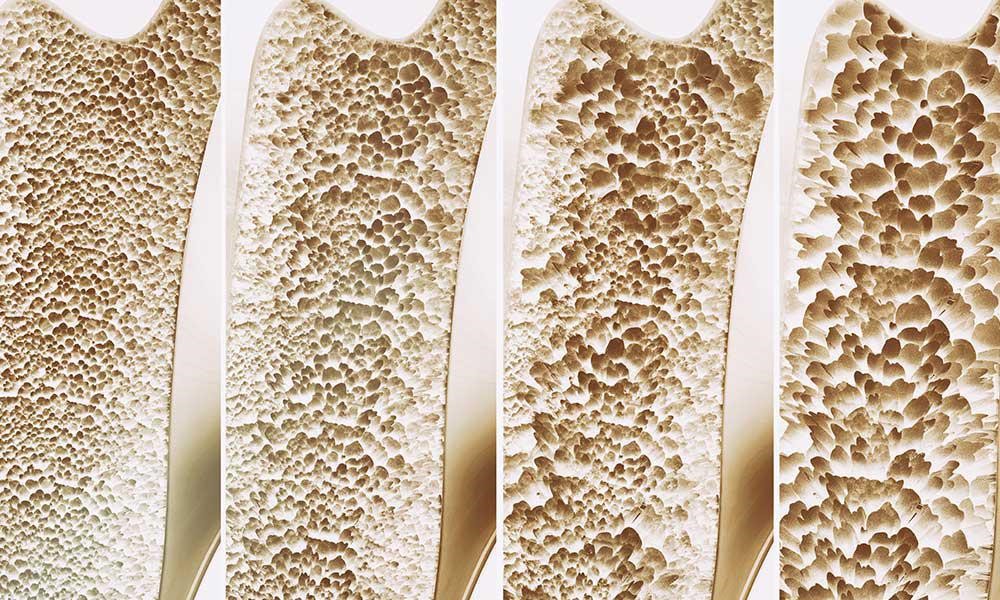
| We all want to avoid elder years of frailty, infirmity, and fractures. But did you know that it is in your power to avoid these common outcomes of old age? Bone health gets little attention in the media, much less than heart health or cancer prevention. But fractures from thin bones are so often the catalyst of infirmity and physical decline. And they are PREVENTABLE! We at Carolina Total Wellness take a comprehensive view of bone health, with the goal of not only stopping bone loss, but actually increasing bone density and quality. This takes a very individual understanding of the many factors that can set us up for bone thinning (osteopenia) or severe bone thinning (osteoporosis). The one we all know is Vitamin D deficiency. But there are so many other impactful nutrients for bones including Vitamin K2, Magnesium, Phosphorus, Boron, and Calcium. And only certain forms of calcium are optimal, as many OTC calcium forms go where we do not want them: our arterial walls, contributing to heart disease and stroke. Milk is NOT a good source of calcium. The increased acidity in the body due to dairy actually sucks out bone mass. Did you know the “Got Milk?” campaign was actually pushed on us by the marketing folks from the cigarette industry after they lost their jobs there? We also know that aging is a factor due to hormonal loss, earlier in women at menopause, but also in men with frequently undiagnosed low testosterone due to many reasons including statin medications, head trauma, or sleep disorders. Optimizing hormones in both men and women Other less recognized factors leading to bone loss that we see often in our practice include chronic inflammation, acidic diets, alcohol use, smoking, and high stress related cortisol levels. Addressing root cause is essential as is careful monitoring of interventions over time. Here is where we would like to introduce you to Dr Andy Bush. He is a board certified Orthopedic Surgeon who says “I used to operate on fractures. Now I want to prevent them.” Please read on for an education in the most cutting edge imaging techniques to monitor bones over time. Osteoporosis – a silent epidemic Andy Bush, MD, Central Carolina Orthopedics, Sanford, NC Rates of osteoporosis and fractures associated with poor bone quality, which are known as fragility fractures, are at epidemic levels. It is estimated that osteoporosis affects approximately 200 million people world-wide. Currently, it is also estimated that 10 million individuals over age 50 in the United States have osteoporosis. Each year an approximately 2 million individuals suffer a fracture due to osteoporosis. The risk of a fracture increases with age and is greatest in women. Approximately 1 in 2 women and 1 and 5 men age 50or older will experience a hip, spine, or wrist fracture sometime during their lives. Approximately 40% of individuals are unable to return to their homes following a fragility fracture and require relocation to a nursing facility. As many as 20% of individuals will die within 6-12 months of a fragility fracture. Also, an additional 33.6 million individuals over age 50 have low bone density or “osteopenia” and thus are at risk of osteoporosis and fragility fracture. Osteoporosis and osteopenia are not painful conditions. Most people are unaware that they have any problems with their bones – that is until that one day when our foot gets caught on the edge of the carpet, or we forgot to wipe up the spilled water on the kitchen floor or our little dog or cat gets in between our feet making us fall and we hear that loud and dreaded “CRACK!!”. Often, after that fateful event, life changes dramatically and then the importance of bone healthcare and not having a healthy skeleton becomes a very painful and life-altering reality. Monitoring of the bone health is the foundation of fracture prevention in the way monitoring blood pressure is to stroke prevention and mammograms are to breast cancer prevention. The early detection of any of these conditions, allows for early treatment to be instituted to prevent the long-term consequences of the disease. Bone health assessment is looking for osteopenia or osteoporosis and determining fracture risk. Although, some may still consider developing osteoporosis an unfortunate part of growing older, it is now understood that fractures due to bone loss are not an inevitable part of aging but a potentially preventable disease process. Nutrition and exercise fight against osteoporosis – monitoring makes sure that they are working. The term for bone monitoring is known as bone densitometry – the measurement of bone density. Determining bone mineral density (BMD) by using Dual Energy X-ray Absorptiometry (DXA) has been the traditional method of diagnosing osteoporosis and predicting fracture risk. It is a method of measuring BMD by using low-energy x-ray and has been considered reasonably reliable for measuring BMD and diagnosing and treating osteoporosis. There is another method of bone densitometry that not only determines BMD but also give a measure of the Bone Quality. Radiofrequency Echographic Multi Spectrometry (REMS) is a newer method of performing monitoring bone health that has been used in Europe for almost a decade and has replaced DXA as the official method of bone densitometry in Italy. REMS uses ultrasound to measure BMD. However, the ultrasound is also capable of measuring Bone Quality and therefore when REMS is used to assess bone, more information is obtained. It is a more reliable method to predict fracture risk. REMS is still very new in the United States but its popularity is growing as more people are learning about it. In conclusion, it is important to remember that your bones need to be monitored and cared for like any other part of you. Bone healthcare is an issue for everyone and something that we all need to be aware of because everyone has a skeleton. And we need to pay attention to and take care of our skeletons because………… If you ignore your bones, they will go away! Your Partner In Health, Frances T Meredith, MD |
 |
Didem Miraloglu, MD, MS
Osteoporosis refers to a condition where bones become brittle. A report from the Surgeon General states in the US 54 million Americans are at risk for osteoporosis, and 10 million Americans already have osteoporosis. Although women make up 80% of osteoporosis cases, men still get osteoporosis. Each year 1.5 million people suffer a fracture from bone loss, and if this is a hip fracture, mortality in the first year can be as high as 40%, with higher mortality rates in men than in women.
Starting in childhood, there is a fine balance between the building up and breaking down of bones coordinated beautifully between cells named osteoblasts and osteoclasts, respectively. If there is too much osteoclast activity, then there is an increased amount of breakdown of bone as seen in inflammation. There is also this misconception that it is the lack of calcium causing osteoporosis. It is actually calcium balance and not the total calcium which is important in osteoporosis.
Risk factors for osteoporosis include:
1) Aging: Inflammation is a normal process of aging, which increases with age, in functional medicine, this is termed “inflamm-aging”.
2) Diet- SAD: Diet (Standard American Diet) is very inflammatory, upregulating the immune system. Consumption of excess amounts of sugar, alcohol, caffeine, salt, and soda all can lead to bone loss due to demineralization of the bones. A leaky gut can drive inflammation to the point of bone resorption.
3) Lifestyle: Stress, smoking, inactive lifestyle can all contribute to an increased rate of breakdown of bone compared to a build-up of bone.
4) Genes: For instance, Celiac disease predisposes to osteoporosis due to poor absorption of minerals.
5) Gender: Being a female increases the risk, since it is usually seen after menopause because estrogen is protective for the bones as well as the brain and the heart. During menopause estrogen declines and there is no further protection for the bones.
6) Medications: Steroids, proton pump inhibitors (omeprazole, pantoprazole, esomeprazole), cancer drugs, thyroid hormone, cyclosporine, heparin, and warfarin.
Testing for osteoporosis is done thru a DEXA scan. It is also known as a Dual Energy X-ray Absorptiometry, or Bone Density scan, a simple X-ray where the hip and the spine bone density are measured. T-score represents the difference in your bone density from the average bone density of healthy young adults. If the T-score is -1 to -2.5 it is considered osteopenia, if <-2.5 osteoporosis. Osteopenia refers to the beginning of osteoporosis, meaning “bone poverty”.
Treatment of osteoporosis by conventional medicine involves using strong drugs, sometimes too strong which may even cause a break in the bones.
1. Bisphosphonates: i.e., Fosamax, Boniva, Actonel, and Reclast target areas of high turnover where the osteoclasts, cells which break down old bone, absorb bisphosphonate and hence their activity is slowed down and there is a reduction in bone breakdown.
Side effects: bone, joint, muscle pain, nausea, gastric ulcer, stress fracture of the thigh bone
2. SERM: Selective estrogen receptor modulator- i.e.Raloxifene, acts like estrogen in some parts of the body but blocks the effects of estrogen in other parts. Increases bone density and reduces the risk of spine fractures, but it has not been shown to decrease the risk of non-spinal fractures. Raloxifene also decreases the risk of invasive breast cancer.
Side effects: hot flashes, leg cramps, or blood clots in the legs or lungs. Raloxifene is not recommended for premenopausal women.
3. Parathyroid hormone molecule: i.e. Teriparatide, abaloparatide stimulates new bone formation, rather than preventing bone breakdown. Because of potential safety concerns, particularly an increased risk of bone cancer in rats, the use of this drug is restricted to men and women with severe osteoporosis—who have a high risk of a fracture—and can be given for no more than two years.
Side effects: uncommon but may include leg cramps, headaches, dizziness, high blood calcium, and high urinary calcium (with an increased risk of kidney stones). This medication is not recommended for premenopausal women.
4. Romosuzumab: Bone-building medication that is given once a month as pair of injections by a doctor or nurse. Treatment is given once a month for twelve months and is then followed by another medication to prevent bone loss. Romosozumab reduces the risk of spine fractures and non-spine fractures, including hip fractures. Romosozumab may increase the risk of heart attack or stroke—including fatal heart attack or stroke—and it should not be given to women who have had a heart attack or stroke in the past year. It is approved for the treatment of osteoporosis in women past the time of menopause who are at high risk for fracture, defined as a history of osteoporotic fracture, multiple risk factors for fracture, or failure or intolerance to other available osteoporosis therapies. It may cause side effects such as headaches or joint pain.
5. Estrogen hormone therapy: Prevents bone loss and reduces the risk of fracture in the spine and hip. It can also relieve other symptoms of menopause, such as hot flashes and vaginal dryness. Estrogen is usually given in pill form, although it is also available in other forms such as a skin patch or gel. Studies show that the risks of oral estrogen therapy—including heart attack, stroke, blood clots, and breast cancer—may outweigh its benefits in many older women, depending upon the dose and specific preparation. For this reason, estrogen therapy is not usually prescribed solely for fracture prevention.
A comprehensive functional medicine approach to the evaluation of osteoporosis takes the form of blood, saliva, stool, and urine testing. Low-grade inflammation can be assessed thru blood work by checking hs-CRP, HgA1C, ESR, CMP, CBC, and essential fatty acids. Blood work for vitamin D and osteocalcin is necessary since vitamin D helps absorb calcium into the bones and osteocalcin is a biomarker for functional vitamin K deficiency. Bone resorption can be evaluated by urine N-telopeptide. Stool analysis to evaluate the gut is also important since calprotectin in stool provides information about inflammation in the gut. Gut microbes are responsible for making vitamin K, which is necessary for having better bone density. Saliva testing for hormones would provide information about the levels of estradiol, testosterone, DHEA, cortisol, and progesterone.
A comprehensive functional medicine approach to the treatment of osteoporosis is first and foremost prevention. It is recommended by conventional doctors to get a DEXA scan once a woman turns 65, however, it may be too late for some since many risk factors play a role in developing osteoporosis. It is ideal to have a DEXA scan around ages 30-35 as a baseline since this is the time of peak bone mass, and then another one a year after menopause to compare the degree of bone loss to get ahead of the condition.
Osteoporosis refers to a condition where bones become brittle. A report from the Surgeon General states in the US 54 million Americans are at risk for osteoporosis, and 10 million Americans already have osteoporosis. Although women make up 80% of osteoporosis cases, men still get osteoporosis. Each year 1.5 million people suffer a fracture from bone loss, and if this is a hip fracture, mortality in the first year can be as high as 40%, with higher mortality rates in men than in women.
Starting in childhood, there is a fine balance between the building up and breaking down of bones coordinated beautifully between cells named osteoblasts and osteoclasts, respectively. If there is too much osteoclast activity, then there is an increased amount of breakdown of bone as seen in inflammation. There is also this misconception that it is the lack of calcium causing osteoporosis. It is actually calcium balance and not the total calcium which is important in osteoporosis.
Risk factors for osteoporosis include:
1) Aging: Inflammation is a normal process of aging, which increases with age, in functional medicine, this is termed “inflamm-aging”.
2) Diet- SAD: Diet (Standard American Diet) is very inflammatory, upregulating the immune system. Consumption of excess amounts of sugar, alcohol, caffeine, salt, and soda all can lead to bone loss due to demineralization of the bones. A leaky gut can drive inflammation to the point of bone resorption.
3) Lifestyle: Stress, smoking, inactive lifestyle can all contribute to an increased rate of breakdown of bone compared to a build-up of bone.
4) Genes: For instance, Celiac disease predisposes to osteoporosis due to poor absorption of minerals.
5) Gender: Being a female increases the risk, since it is usually seen after menopause because estrogen is protective for the bones as well as the brain and the heart. During menopause estrogen declines and there is no further protection for the bones.
6) Medications: Steroids, proton pump inhibitors (omeprazole, pantoprazole, esomeprazole), cancer drugs, thyroid hormone, cyclosporine, heparin, and warfarin.
Testing for osteoporosis is done thru a DEXA scan. It is also known as a Dual Energy X-ray Absorptiometry, or Bone Density scan, a simple X-ray where the hip and the spine bone density are measured. T-score represents the difference in your bone density from the average bone density of healthy young adults. If the T-score is -1 to -2.5 it is considered osteopenia, if <-2.5 osteoporosis. Osteopenia refers to the beginning of osteoporosis, meaning “bone poverty”.
Treatment of osteoporosis by conventional medicine involves using strong drugs, sometimes too strong which may even cause a break in the bones.
1. Bisphosphonates: i.e., Fosamax, Boniva, Actonel, and Reclast target areas of high turnover where the osteoclasts, cells which break down old bone, absorb bisphosphonate and hence their activity is slowed down and there is a reduction in bone breakdown.
Side effects: bone, joint, muscle pain, nausea, gastric ulcer, stress fracture of the thigh bone
2. SERM: Selective estrogen receptor modulator- i.e.Raloxifene, acts like estrogen in some parts of the body but blocks the effects of estrogen in other parts. Increases bone density and reduces the risk of spine fractures, but it has not been shown to decrease the risk of non-spinal fractures. Raloxifene also decreases the risk of invasive breast cancer.
Side effects: hot flashes, leg cramps, or blood clots in the legs or lungs. Raloxifene is not recommended for premenopausal women.
3. Parathyroid hormone molecule: i.e. Teriparatide, abaloparatide stimulates new bone formation, rather than preventing bone breakdown. Because of potential safety concerns, particularly an increased risk of bone cancer in rats, the use of this drug is restricted to men and women with severe osteoporosis—who have a high risk of a fracture—and can be given for no more than two years.
Side effects: uncommon but may include leg cramps, headaches, dizziness, high blood calcium, and high urinary calcium (with an increased risk of kidney stones). This medication is not recommended for premenopausal women.
4. Romosuzumab: Bone-building medication that is given once a month as pair of injections by a doctor or nurse. Treatment is given once a month for twelve months and is then followed by another medication to prevent bone loss. Romosozumab reduces the risk of spine fractures and non-spine fractures, including hip fractures. Romosozumab may increase the risk of heart attack or stroke—including fatal heart attack or stroke—and it should not be given to women who have had a heart attack or stroke in the past year. It is approved for the treatment of osteoporosis in women past the time of menopause who are at high risk for fracture, defined as a history of osteoporotic fracture, multiple risk factors for fracture, or failure or intolerance to other available osteoporosis therapies. It may cause side effects such as headaches or joint pain.
5. Estrogen hormone therapy: Prevents bone loss and reduces the risk of fracture in the spine and hip. It can also relieve other symptoms of menopause, such as hot flashes and vaginal dryness. Estrogen is usually given in pill form, although it is also available in other forms such as a skin patch or gel. Studies show that the risks of oral estrogen therapy—including heart attack, stroke, blood clots, and breast cancer—may outweigh its benefits in many older women, depending upon the dose and specific preparation. For this reason, estrogen therapy is not usually prescribed solely for fracture prevention.
A comprehensive functional medicine approach to the evaluation of osteoporosis takes the form of blood, saliva, stool, and urine testing. Low-grade inflammation can be assessed thru blood work by checking hs-CRP, HgA1C, ESR, CMP, CBC, and essential fatty acids. Blood work for vitamin D and osteocalcin is necessary since vitamin D helps absorb calcium into the bones and osteocalcin is a biomarker for functional vitamin K deficiency. Bone resorption can be evaluated by urine N-telopeptide. Stool analysis to evaluate the gut is also important since calprotectin in stool provides information about inflammation in the gut. Gut microbes are responsible for making vitamin K, which is necessary for having better bone density. Saliva testing for hormones would provide information about the levels of estradiol, testosterone, DHEA, cortisol, and progesterone.
A comprehensive functional medicine approach to the treatment of osteoporosis is first and foremost prevention. It is recommended by conventional doctors to get a DEXA scan once a woman turns 65, however, it may be too late for some since many risk factors play a role in developing osteoporosis. It is ideal to have a DEXA scan around ages 30-35 as a baseline since this is the time of peak bone mass, and then another one a year after menopause to compare the degree of bone loss to get ahead of the condition.
Once you have osteoporosis then the treatment is as follows:
Your partner in health,
Didem Miraloglu, MD, MS

Functional medicine is a science-based health care approach to assess, prevent and treat complex chronic disease.
![]() Learn More
Learn More
After a brief allergy test, you can begin sublingual immunotherapy (SLIT), or allergy drops under the tongue. No more allergy shots!
![]() Learn More
Learn More
Learn how to prepare for your visit and what to expect at your initial consultation and at your follow-up visits with our office.
![]() Learn More
Learn More