For many individuals diagnosed with Candida, guidance on the Candida diet—and its role in managing and preventing yeast overgrowth—is often overlooked. Here, at Carolina Total Wellness, we combine medications and supplements with personalized guidance to help our patients successfully navigate the Candida diet.
In a healthy system, Candida coexists with other microorganisms in the gut, mouth, and skin. However, when it grows excessively—often triggered by factors such as antibiotic use, high sugar intake, stress, or a weakened immune system—it can lead to a condition known as candidiasis.
Symptoms may include digestive discomfort, fatigue, brain fog, recurring infections, or skin issues. The goal of the Candida diet is to restore microbial balance by depriving yeast of its preferred food sources and promoting the growth of beneficial bacteria.
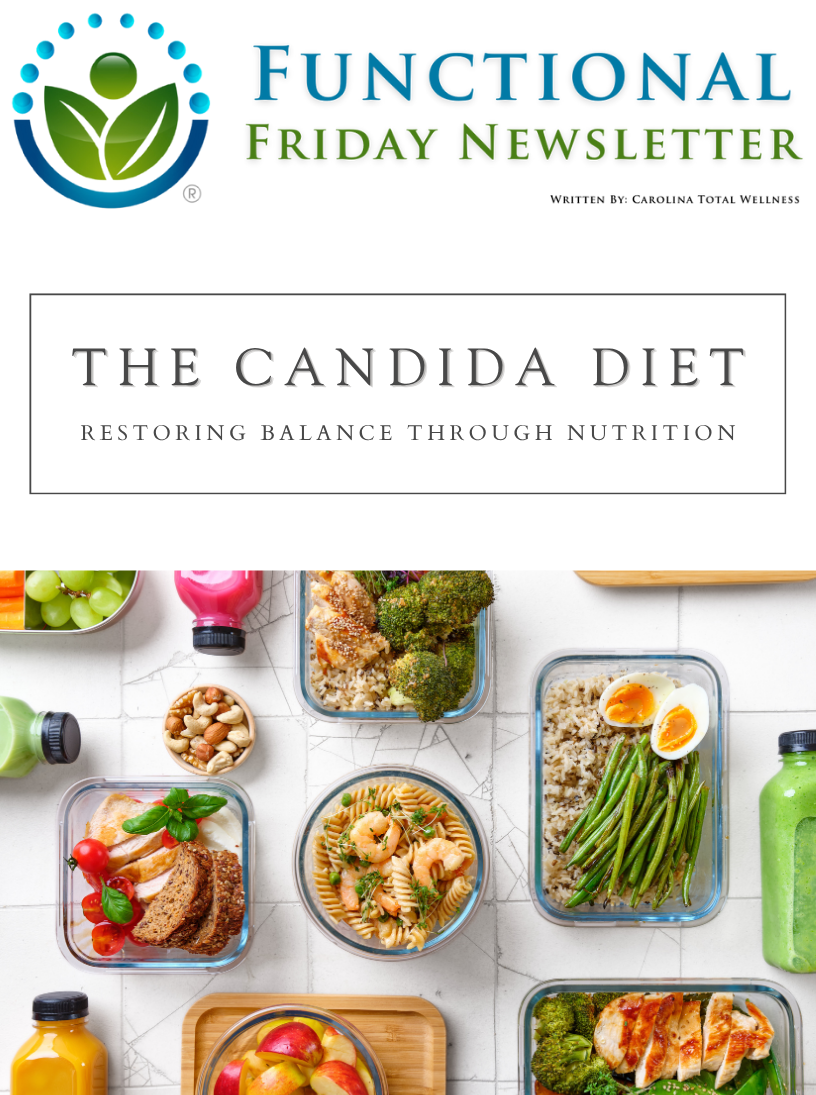
At its core, the Candida diet emphasizes whole, unprocessed, and low-sugar foods while eliminating ingredients that feed yeast or irritate the gut. Sugar—whether refined, natural, or artificial—is strictly limited because Candida thrives on glucose.
Key components of the Candida diet include high-quality protein sources, such as poultry, fish, eggs, certain plant-based proteins, and non-glutinous grains.
Healthy fats from avocados, olive oil, and coconut oil help stabilize blood sugar and support cellular repair.
Non-starchy vegetables—including leafy greens, broccoli, cauliflower, zucchini, and cucumbers—provide essential fiber and antioxidants that nourish beneficial gut bacteria and assist detoxification.
Equally important is avoiding foods that encourage yeast proliferation. These include sugar in all forms (including honey and maple syrup), white flour, alcohol, and high-carbohydrate foods such as potatoes, corn, and most grains. Fermented foods like vinegar, kombucha, and soy sauce are often restricted, as they may contribute to histamine buildup or trigger sensitivities during the initial healing phase.
The Candida diet also encourages gut restoration through probiotics and prebiotic foods. Probiotic supplements or naturally cultured foods like unsweetened yogurt and kefir (if tolerated) help replenish beneficial bacteria that keep Candida in check.
Adequate hydration, stress management, and proper sleep are additional pillars of success, since the immune system plays a crucial role in maintaining microbial balance.
While the Candida diet can be restrictive, many people report improved digestion, energy, and mental clarity after several weeks. Expert guidance from our team at Carolina Total Wellness helps you follow the Candida diet safely to restore gut balance and long-term wellness.