
Follow us on Social Media!
 919-999-0831
919-999-0831

Follow us on Social Media!
Follow Carolina Total Wellness on Social Media!


The hormonal shifts that accompany perimenopause and menopause lack a clear instruction manual, often leaving many women in a continuous cycle of trial and error when it comes to managing their symptoms. Fortunately, one of the most potent tools available for regaining control of your hormones is the food you consume. Certain foods contribute to hormone balance and can help alleviate perimenopause and menopause symptoms, while others can disrupt your body’s hormonal equilibrium.
When essential nutritional elements are lacking, hormonal imbalances can arise, leading to mood swings, weight gain, hot flashes, and reduced libido. The primary hormones affected during perimenopause and menopause are estrogen, progesterone, insulin, and testosterone, and your dietary choices can significantly impact these hormones. For instance, excessive sugar consumption can elevate insulin levels, trigger inflammation, and exacerbate nearly every perimenopausal symptom. On the other hand, incorporating vegetables, fruits, nuts, and seeds into your diet can provide phytonutrients and healthy fats that aid in managing even the most challenging menopause symptoms.
While there’s no one-size-fits-all diet, several foods have proven beneficial for most people seeking to balance their hormones:
1. Brassica (aka cruciferous) Vegetables: These include broccoli, cauliflower, kale, and cabbage, which contain indole-3-carbinol—a compound that helps metabolize estrogen in the gut and liver. This can be particularly helpful in addressing estrogen dominance.
2. Healthy Fats: Avocados, nuts, seeds, and fish are rich inomega-3 fatty acids and other fats crucial for reducing inflammation and supporting hormone production, especially progesterone.
3. Fiber-Rich Foods: Fiber is essential for gut health, which plays a critical role in hormone balance. Low-starch fruits and veggies, nuts, seeds, and whole grains can boost your fiber intake, aiding in estrogen metabolism and blood sugar regulation.
However, there are also foods and drinks that should be limited or avoided:
1. Caffeine: Excess caffeine can lead to increased stress hormone production and elevated cortisol levels, potentially exacerbating fatigue and estrogen levels.
2. Processed Carbs and Sugar: As tolerance to sugar decreases with age, limiting simple carbohydrates and sugars (like table sugar, baked goods, and packaged foods) becomes crucial for managing blood sugar and insulin levels.
3. Alcohol: Even moderate alcohol consumption can disrupt hormones, affect brain aging, and lead to elevated insulin levels and estrogen dominance.
4. Gluten: Gluten sensitivity can contribute to gut issues, thyroid problems, and autoimmune conditions, making it advisable to assess its impact on your health
Balancing your diet can ease the transition into perimenopause and menopause, regardless of whether you’re just beginning to experience symptoms or are already in the midst of them. By making thoughtful dietary choices, you can navigate this phase of life with greater vitality and well-being.
Your Partner In Health,
Sara Yadlowsky, FMHC
Sara Yadlowsky, FMHC
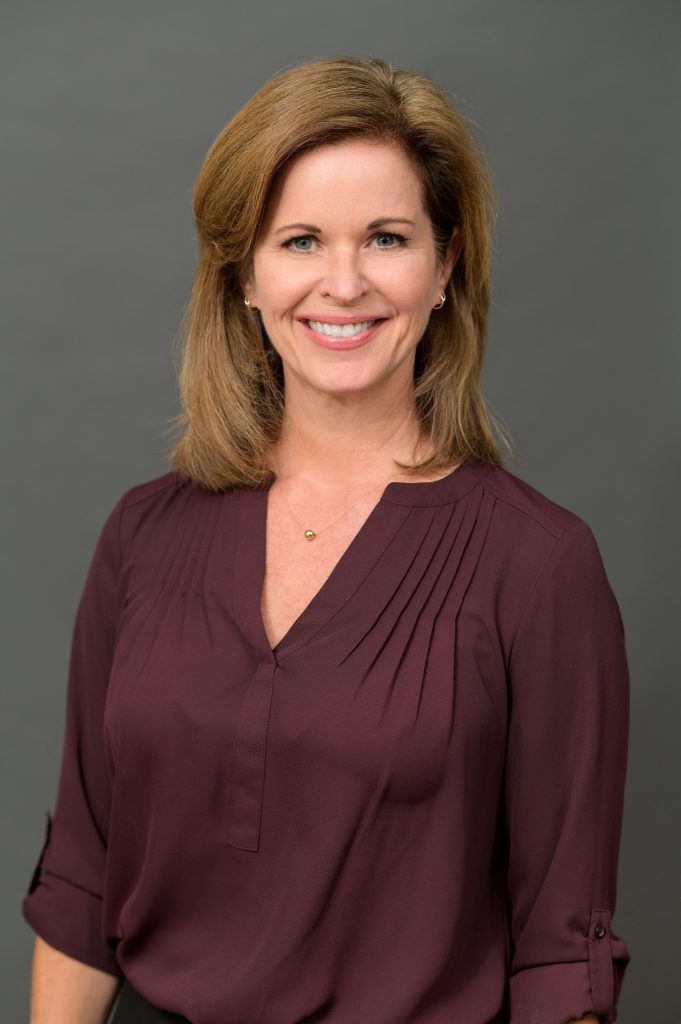
What doesn’t kill you makes you stronger. We’ve all heard the saying before. Science has revealed it is surprisingly accurate when it comes to our health and longevity.
Hormesis is the idea that short, intermittent bursts of certain stressors can start a cascade of cellular processes that slow aging, improve overall health and make you more resilient, both physically and mentally. It is a hot topic in longevity research right now.
We all know that chronic stress caused by relationship issues, financial problems and working too many hours is detrimental to our health. However, hormetic stressors are controlled and acute, triggering healthy adaptive responses.
What does all this mean in real life? Hormesis is the common thread found in some popular health and fitness trends such as HIIT (high intensity interval training), cold exposure, heat therapy and intermittent fasting. Prolonged doses of these behaviors are not healthy or sustainable. For example, if you spend too much time in a sauna you will become dehydrated. But, in short bursts, the bodily stress caused by these practices are enough to bring about health benefits such as reducing inflammation, supporting elimination of toxins, repairing DNA, combatting oxidative stress, repairing cellular damage and reducing risk of cancer.
Here are three ways to strategically stress your body and reap the rewards:
Be aware that adding stress (even the good type!) to our lives can backfire if done at the wrong time. When life is already very stressful, it is best to wait until a better time when you are more relaxed to try out these new practices.
Your Partner In Health,
Sara Yadlowsky, FMHC
Didem Miraloglu, MD, MS
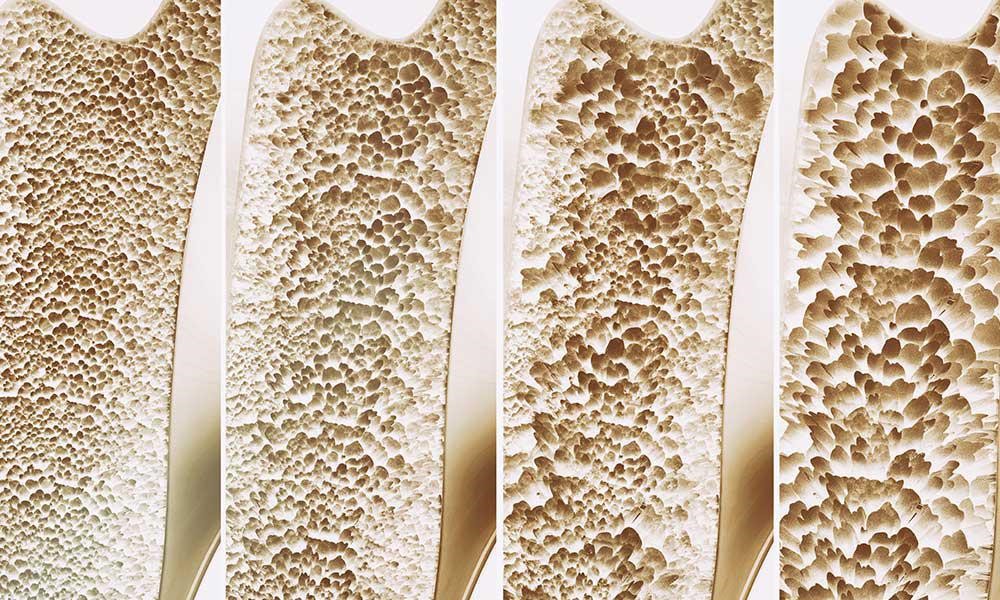
Osteoporosis refers to a condition where bones become brittle. A report from the Surgeon General states in the US 54 million Americans are at risk for osteoporosis, and 10 million Americans already have osteoporosis. Although women make up 80% of osteoporosis cases, men still get osteoporosis. Each year 1.5 million people suffer a fracture from bone loss, and if this is a hip fracture, mortality in the first year can be as high as 40%, with higher mortality rates in men than in women.
Starting in childhood, there is a fine balance between the building up and breaking down of bones coordinated beautifully between cells named osteoblasts and osteoclasts, respectively. If there is too much osteoclast activity, then there is an increased amount of breakdown of bone as seen in inflammation. There is also this misconception that it is the lack of calcium causing osteoporosis. It is actually calcium balance and not the total calcium which is important in osteoporosis.
Risk factors for osteoporosis include:
1) Aging: Inflammation is a normal process of aging, which increases with age, in functional medicine, this is termed “inflamm-aging”.
2) Diet- SAD: Diet (Standard American Diet) is very inflammatory, upregulating the immune system. Consumption of excess amounts of sugar, alcohol, caffeine, salt, and soda all can lead to bone loss due to demineralization of the bones. A leaky gut can drive inflammation to the point of bone resorption.
3) Lifestyle: Stress, smoking, inactive lifestyle can all contribute to an increased rate of breakdown of bone compared to a build-up of bone.
4) Genes: For instance, Celiac disease predisposes to osteoporosis due to poor absorption of minerals.
5) Gender: Being a female increases the risk, since it is usually seen after menopause because estrogen is protective for the bones as well as the brain and the heart. During menopause estrogen declines and there is no further protection for the bones.
6) Medications: Steroids, proton pump inhibitors (omeprazole, pantoprazole, esomeprazole), cancer drugs, thyroid hormone, cyclosporine, heparin, and warfarin.
Testing for osteoporosis is done thru a DEXA scan. It is also known as a Dual Energy X-ray Absorptiometry, or Bone Density scan, a simple X-ray where the hip and the spine bone density are measured. T-score represents the difference in your bone density from the average bone density of healthy young adults. If the T-score is -1 to -2.5 it is considered osteopenia, if <-2.5 osteoporosis. Osteopenia refers to the beginning of osteoporosis, meaning “bone poverty”.
Treatment of osteoporosis by conventional medicine involves using strong drugs, sometimes too strong which may even cause a break in the bones.
1. Bisphosphonates: i.e., Fosamax, Boniva, Actonel, and Reclast target areas of high turnover where the osteoclasts, cells which break down old bone, absorb bisphosphonate and hence their activity is slowed down and there is a reduction in bone breakdown.
Side effects: bone, joint, muscle pain, nausea, gastric ulcer, stress fracture of the thigh bone
2. SERM: Selective estrogen receptor modulator- i.e.Raloxifene, acts like estrogen in some parts of the body but blocks the effects of estrogen in other parts. Increases bone density and reduces the risk of spine fractures, but it has not been shown to decrease the risk of non-spinal fractures. Raloxifene also decreases the risk of invasive breast cancer.
Side effects: hot flashes, leg cramps, or blood clots in the legs or lungs. Raloxifene is not recommended for premenopausal women.
3. Parathyroid hormone molecule: i.e. Teriparatide, abaloparatide stimulates new bone formation, rather than preventing bone breakdown. Because of potential safety concerns, particularly an increased risk of bone cancer in rats, the use of this drug is restricted to men and women with severe osteoporosis—who have a high risk of a fracture—and can be given for no more than two years.
Side effects: uncommon but may include leg cramps, headaches, dizziness, high blood calcium, and high urinary calcium (with an increased risk of kidney stones). This medication is not recommended for premenopausal women.
4. Romosuzumab: Bone-building medication that is given once a month as pair of injections by a doctor or nurse. Treatment is given once a month for twelve months and is then followed by another medication to prevent bone loss. Romosozumab reduces the risk of spine fractures and non-spine fractures, including hip fractures. Romosozumab may increase the risk of heart attack or stroke—including fatal heart attack or stroke—and it should not be given to women who have had a heart attack or stroke in the past year. It is approved for the treatment of osteoporosis in women past the time of menopause who are at high risk for fracture, defined as a history of osteoporotic fracture, multiple risk factors for fracture, or failure or intolerance to other available osteoporosis therapies. It may cause side effects such as headaches or joint pain.
5. Estrogen hormone therapy: Prevents bone loss and reduces the risk of fracture in the spine and hip. It can also relieve other symptoms of menopause, such as hot flashes and vaginal dryness. Estrogen is usually given in pill form, although it is also available in other forms such as a skin patch or gel. Studies show that the risks of oral estrogen therapy—including heart attack, stroke, blood clots, and breast cancer—may outweigh its benefits in many older women, depending upon the dose and specific preparation. For this reason, estrogen therapy is not usually prescribed solely for fracture prevention.
A comprehensive functional medicine approach to the evaluation of osteoporosis takes the form of blood, saliva, stool, and urine testing. Low-grade inflammation can be assessed thru blood work by checking hs-CRP, HgA1C, ESR, CMP, CBC, and essential fatty acids. Blood work for vitamin D and osteocalcin is necessary since vitamin D helps absorb calcium into the bones and osteocalcin is a biomarker for functional vitamin K deficiency. Bone resorption can be evaluated by urine N-telopeptide. Stool analysis to evaluate the gut is also important since calprotectin in stool provides information about inflammation in the gut. Gut microbes are responsible for making vitamin K, which is necessary for having better bone density. Saliva testing for hormones would provide information about the levels of estradiol, testosterone, DHEA, cortisol, and progesterone.
A comprehensive functional medicine approach to the treatment of osteoporosis is first and foremost prevention. It is recommended by conventional doctors to get a DEXA scan once a woman turns 65, however, it may be too late for some since many risk factors play a role in developing osteoporosis. It is ideal to have a DEXA scan around ages 30-35 as a baseline since this is the time of peak bone mass, and then another one a year after menopause to compare the degree of bone loss to get ahead of the condition.
Osteoporosis refers to a condition where bones become brittle. A report from the Surgeon General states in the US 54 million Americans are at risk for osteoporosis, and 10 million Americans already have osteoporosis. Although women make up 80% of osteoporosis cases, men still get osteoporosis. Each year 1.5 million people suffer a fracture from bone loss, and if this is a hip fracture, mortality in the first year can be as high as 40%, with higher mortality rates in men than in women.
Starting in childhood, there is a fine balance between the building up and breaking down of bones coordinated beautifully between cells named osteoblasts and osteoclasts, respectively. If there is too much osteoclast activity, then there is an increased amount of breakdown of bone as seen in inflammation. There is also this misconception that it is the lack of calcium causing osteoporosis. It is actually calcium balance and not the total calcium which is important in osteoporosis.
Risk factors for osteoporosis include:
1) Aging: Inflammation is a normal process of aging, which increases with age, in functional medicine, this is termed “inflamm-aging”.
2) Diet- SAD: Diet (Standard American Diet) is very inflammatory, upregulating the immune system. Consumption of excess amounts of sugar, alcohol, caffeine, salt, and soda all can lead to bone loss due to demineralization of the bones. A leaky gut can drive inflammation to the point of bone resorption.
3) Lifestyle: Stress, smoking, inactive lifestyle can all contribute to an increased rate of breakdown of bone compared to a build-up of bone.
4) Genes: For instance, Celiac disease predisposes to osteoporosis due to poor absorption of minerals.
5) Gender: Being a female increases the risk, since it is usually seen after menopause because estrogen is protective for the bones as well as the brain and the heart. During menopause estrogen declines and there is no further protection for the bones.
6) Medications: Steroids, proton pump inhibitors (omeprazole, pantoprazole, esomeprazole), cancer drugs, thyroid hormone, cyclosporine, heparin, and warfarin.
Testing for osteoporosis is done thru a DEXA scan. It is also known as a Dual Energy X-ray Absorptiometry, or Bone Density scan, a simple X-ray where the hip and the spine bone density are measured. T-score represents the difference in your bone density from the average bone density of healthy young adults. If the T-score is -1 to -2.5 it is considered osteopenia, if <-2.5 osteoporosis. Osteopenia refers to the beginning of osteoporosis, meaning “bone poverty”.
Treatment of osteoporosis by conventional medicine involves using strong drugs, sometimes too strong which may even cause a break in the bones.
1. Bisphosphonates: i.e., Fosamax, Boniva, Actonel, and Reclast target areas of high turnover where the osteoclasts, cells which break down old bone, absorb bisphosphonate and hence their activity is slowed down and there is a reduction in bone breakdown.
Side effects: bone, joint, muscle pain, nausea, gastric ulcer, stress fracture of the thigh bone
2. SERM: Selective estrogen receptor modulator- i.e.Raloxifene, acts like estrogen in some parts of the body but blocks the effects of estrogen in other parts. Increases bone density and reduces the risk of spine fractures, but it has not been shown to decrease the risk of non-spinal fractures. Raloxifene also decreases the risk of invasive breast cancer.
Side effects: hot flashes, leg cramps, or blood clots in the legs or lungs. Raloxifene is not recommended for premenopausal women.
3. Parathyroid hormone molecule: i.e. Teriparatide, abaloparatide stimulates new bone formation, rather than preventing bone breakdown. Because of potential safety concerns, particularly an increased risk of bone cancer in rats, the use of this drug is restricted to men and women with severe osteoporosis—who have a high risk of a fracture—and can be given for no more than two years.
Side effects: uncommon but may include leg cramps, headaches, dizziness, high blood calcium, and high urinary calcium (with an increased risk of kidney stones). This medication is not recommended for premenopausal women.
4. Romosuzumab: Bone-building medication that is given once a month as pair of injections by a doctor or nurse. Treatment is given once a month for twelve months and is then followed by another medication to prevent bone loss. Romosozumab reduces the risk of spine fractures and non-spine fractures, including hip fractures. Romosozumab may increase the risk of heart attack or stroke—including fatal heart attack or stroke—and it should not be given to women who have had a heart attack or stroke in the past year. It is approved for the treatment of osteoporosis in women past the time of menopause who are at high risk for fracture, defined as a history of osteoporotic fracture, multiple risk factors for fracture, or failure or intolerance to other available osteoporosis therapies. It may cause side effects such as headaches or joint pain.
5. Estrogen hormone therapy: Prevents bone loss and reduces the risk of fracture in the spine and hip. It can also relieve other symptoms of menopause, such as hot flashes and vaginal dryness. Estrogen is usually given in pill form, although it is also available in other forms such as a skin patch or gel. Studies show that the risks of oral estrogen therapy—including heart attack, stroke, blood clots, and breast cancer—may outweigh its benefits in many older women, depending upon the dose and specific preparation. For this reason, estrogen therapy is not usually prescribed solely for fracture prevention.
A comprehensive functional medicine approach to the evaluation of osteoporosis takes the form of blood, saliva, stool, and urine testing. Low-grade inflammation can be assessed thru blood work by checking hs-CRP, HgA1C, ESR, CMP, CBC, and essential fatty acids. Blood work for vitamin D and osteocalcin is necessary since vitamin D helps absorb calcium into the bones and osteocalcin is a biomarker for functional vitamin K deficiency. Bone resorption can be evaluated by urine N-telopeptide. Stool analysis to evaluate the gut is also important since calprotectin in stool provides information about inflammation in the gut. Gut microbes are responsible for making vitamin K, which is necessary for having better bone density. Saliva testing for hormones would provide information about the levels of estradiol, testosterone, DHEA, cortisol, and progesterone.
A comprehensive functional medicine approach to the treatment of osteoporosis is first and foremost prevention. It is recommended by conventional doctors to get a DEXA scan once a woman turns 65, however, it may be too late for some since many risk factors play a role in developing osteoporosis. It is ideal to have a DEXA scan around ages 30-35 as a baseline since this is the time of peak bone mass, and then another one a year after menopause to compare the degree of bone loss to get ahead of the condition.
Once you have osteoporosis then the treatment is as follows:
Your partner in health,
Didem Miraloglu, MD, MS

Sara Yadlowsky, FMHC

Many of us have too much glucose (blood sugar) in our system and are not aware of it. Glucose enters our bloodstream mainly through the sweet or starchy foods we eat. The conventional medicine community has taught for many years that unless you are diabetic or pre-diabetic your blood sugar levels are not important. However, more recent, cutting-edge science and the increased use of continuous glucose monitors (CGM’s) have proven that everyone needs to pay more attention to glucose levels. A CGM is a small device that attaches to the back of your arm and monitors blood glucose on a continuous basis. You can obtain a CGM through a prescription or purchase one online through websites such as Signos, Veri and Nutrisense. I wore a CGM for several weeks recently and found it very informative in understanding how my food choices affect my blood sugar levels. For example, I realized how breaking my fast with a low carb meal was very helpful in avoiding the spike that can occur after fasting for 16 hours.
Symptoms of uncontrolled glucose can include fatigue, food cravings and brain fog. Long term effects of uncontrolled glucose can include hormonal dysfunction, acne, wrinkles and infertility. Over time the development of type 2 diabetes, cancer, dementia, PCOS and heart disease can occur.
There are several easy modifications you can make to your diet that flatten the glucose curve that occurs after eating. These modifications include:
There is a new book out about blood glucose called The Glucose Revolution written by Jessie Inchauspe. The author goes into depth about the huge impact glucose has on our health. She then presents several ways to control our blood sugar more effectively. The book also includes tips on how to handle cravings, better choices in alcohol and how to read ingredient labels.
Jessie Inchauspe has an Instagram account (glucosegoddess) that continues the education on controlling glucose and gives lots of actional advice. This may help provide you with some motivation to jump start a healthier lifestyle in 2023. Our health coaches and physicians at Carolina Total Wellness are also always available to provide you with personalized advice on improved blood sugar control.
In health,
Sara Yadlowsky, FMHC


 |
| Functional Fertility: Basics and Beyond for Pre-conception Whether trying to conceive naturally or going through advanced reproductive options, there are lifestyle, nutritional, nutraceutical and botanical interventions to support optimal fertility. We need balanced hormone communication and low levels of inflammation for a woman’s body to create and nourish new life. There are major leverage points for understanding your body’s baseline of communication and inflammation. These include the Basics: checking in with your sleep quality and daily nutrient intake; and Beyond: testing for personalized understanding of your hormonal health, nutrient needs and inflammatory status. Basics: Some quality Zzzs… Good sleep hygiene is important for our general restoration, healing and detoxification. Our daily circadian rhythm should be an appropriate balance of our stress hormone cortisol, and our restorative hormone, melatonin. Related to healthy menstrual cycles, chronic low overnight melatonin impacts hormone signaling between the brain and ovaries. Hormones necessary for conception include luteinizing hormone (LH), estrogen and progesterone. Production of these hormones is decreased in chronic low melatonin levels. Melatonin is an important antioxidant in the follicular fluid ovarian eggs are swimming in. It acts as a strong scavenger of free radicals, protecting egg cells from cellular damage. Melatonin is also anti-inflammatory, turning down cranky messengers like NF-KB and turning up calming ones like IL-4 and IL-10. Studies with IVF patients taking even 3mg of melatonin nightly days 5 until mid-cycle showed a 4-fold increase in follicular melatonin, which resulted in decreased oxidative damage of these eggs and higher pregnancy rates. Regular sleep is key for fertility. Aim for 8 hours nightly and turn off screens at least one hour before bedtime. This is to address not only the blue light impact on wakefulness, but also to limit the cognitive and psychological stimulation from texting and scrolling through feeds, for example. Use the later hours in the day to turn your attention inward and cultivate, rather than demand, sleep. Consider breathing exercises, calming herbal teas including chamomile and lemon balm, gratitude journaling and yoga nidra. Step away from the chicken fried biscuit…. When examining your nutrient intake, if you need a template to guide changes, I recommend the Mediterranean food plan. It has shown to improve markers of fertility for females and males. Its major principles include: Emphasis on fruits and vegetables, providing great phytonutrient and antioxidant diversity Higher content of omega 3 fatty acids, which are anti-inflammatory, support cell membranes and improve blood viscosity which ensures good blood flow to the uterus Mediterranean foods are rich in B6 and folate – fertility boosting nutrients! Dietary fiber from vegetables and grains – keeps bowels moving regularly to support healthy detox to mobilize toxins and hormone metabolites like high estrogen, high cortisol. Beyond: How’s my thyroid doing? Low thyroid function affects fertility. Around 1/3 of women experiencing subfertility have thyroid disease. The ovaries and egg cells have receptors for thyroid hormone. Thyroid testing includes TSH, free T4, free T3. TSH levels <3 are associated with better ovarian reserve. It’s important to also consider antibodies to the thyroid. Even in a patient with normal thyroid levels, presence of thyroid antibodies is correlated to increased rates of miscarriage and pregnancy-related complications. What’s my Vitamin D level? Vitamin D deficiency is linked to a number of reproductive issues, including gestational diabetes, endometriosis and PCOS. Vitamin D levels >30ng/mL are associated with greater rates of pregnancy. This is likely due to higher levels of anti-mullerian hormone (AMH) when vitamin D is sufficient. The more AMH, the more eggs in the ovarian reserve, the more changes for successful pregnancy. Vitamin D is also involved in helping create endometrial docking sites to help an embryo attach and hold on tight! What’s my iron status? Iron deficiency is common in subfertility. Iron’s job is to deliver oxygen to tissues throughout the body, including the uterus and ovaries. Chronic oxygen deprivation can take a toll on egg quality and result in anovulation. Adequate iron levels build a nice, fluffy endometrium…a cozy place for an embryo to attach. Am I inflamed, you ask? A balanced immune system is important in order to conceive and carry pregnancy to term. One’s general level of inflammation can be assessed with the blood test, hs-CRP. Contributors to systemic inflammation include gum disease, food sensitivities, insulin resistance and imbalances in gut microbiome. Nutrients and botanicals to help reduce inflammation include omega 3s (fish oil) and curcumin. Additional testing is available to further investigate these areas of potential inflammation if needed. Help your cup “run-eth” over With all things, give yourself grace and start from a place of fullness. Know that you are enough! By integrating supports to reduce inflammation and balance communication, your internal supports will overflow to support the life of another. Fill your body with adequate sleep, nutrients, love, support and confidence! Your Partner In Health! Blair Cuneo, PA-C |

1. Butter
It is a very common fat that everybody has (or should have from now on) in their fridge. As opposed to industrial trans fat, which increases the the risk of heart disease, the trans-rumenic acid called conjugated linoleic acid (CLA) is thought to decrease the risk for cardiovescular disease. CLA along with other natural trans fats as well as vitamin K2 are abundantly found in grass-fed meat and dairy products, which is why butter is a great source to maintain cardiovescular health and to prevent heart attacks.
2. Coconut Oil
Coconut oil currently has gained in popularity for all kinds of health remedies and benefits. The hype is justified and it definitely belongs in the kitchen and on this list! First of all, coconut oil is one of the best oils to cook with as it is with more than 90% almost entirely saturated. Its chemical structure stands out to other fats and oils in our diet, which has a significant effect on the body and the heart. Coconut oil is composed of a special type of saturated fat called medium chain triglyceride (MCT). This structure makes the oil special because the vast majority of fats and oils we consume are composed of long-chain fatty acids (LCFA). In fact, both the saturated and unsaturated fat found in meat, eggs, milk, and plants consist of LCFA.
That means that most of the western world gets way too much of these fats and not enough of the MCFA’s that are found in coconut oil.
Why does that matter? Because of its shorter chemical composition, MCFA’s are absorbed with ease without requiring pancreatic enzymes to break them down. This means less work for the pancreas and the fatty acids can go directly to the liver from where they go into the mitochondrias and are immediately utilized for energy. The best part is that coconut oil makes our heart happy by protecting it from heart disease as well as lowering the risk of atherosclerosis.
3. Duck Fat
Just like butter, duck fat is packed with the favorable CLA’s and natural trans fat that were found, in animal studies, to prevent fatty streaks and plaque formation in the arteries of rodents by changing macrophage lipid metabolism.
Another statistic, however, shows that the same effect seems to apply for humans as well. According to the World Health Organization’s Multinational Monitoring of Trends and Determinants, in the United States, of every 100,000 middle-aged men, 315 die of heart attacks each year. However, in the Gascony region, where duck liver is a steady part of the diet, this rate is only 80 per 100,000. A great statistic for the consumption of duck fat and the relation to a healthier heart!
4. Leaf Lard
This fat is a highly popular fat in the kitchen of every celebrity cook. For good reason! Lard is a very stable fat which makes it an excellent choice for frying. Morover, it has a higher smoking point than other fats therefore it is excellent for cooking in general. It is gained from the visceral fat deposit that surrounds the kidney and loin and because of its little pork flavor, leaf lard is considered the highest grade of lard.
Nutritionally speaking, lard is composed of more than twice the monosaturated fat and nearly one-fourth the saturated fat than butter. In addition to that, it is also low in omega-6 fatty acids, known to promote inflammation, which is good news for a healthy heart.
5. Ghee
Ghee, a great fat for cooking, taste, and cardiovescular health. It is made from butter, however, the milk solids and impurities are removed, which makes it consumer friendly for everybody, including people who are lactose or casein intolerant.
Just like coconut oil, it is composed of medium chain fatty acids (MCFA), which are directly absorbed to the liver and burned as energy. Besides of being a fabulous energy source, it contributes to a healthy heart as it protects the arteries from hardening. A study from 2010 found that people in India, where ghee is originated from and thus has the highest population of consumers, had fewer cases of heart disease than our western world.
Sister Act: The Story of E&P
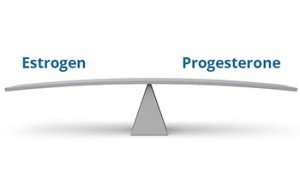
We are all trying to seek balance and the systems in our body are no different, particularly our hormonal system. The differences between the many hormones in our bodies and the roles they play are meant to balance each other. This ying and yang is beautiful and important! Sure, there may be an appropriate time for one hormone to be in abundance, but not all the time. The consequences of imbalance are felt in our bodies, brains and by our loved ones sometimes! And unfortunately, when we do reach out for help, there can be misunderstanding, misdiagnosis and totally missing the mark on root cause.
Today we focus on the dance between estrogen and progesterone in our menstrual cycles and what happens when balance is lost. There is a natural shift over time, but the way we live, what we eat, the products we use in our home, and imbalance in our microbiome and detox health can speed up and intensify the process.
Mood changes, sleep disruption, menstrual cycle changes, nothing’s off limits. Today we hope to empower you with the knowledge of understanding the typical hormone timeline, recognizing signs your body may be sending to warn you and what tools to implement to find your balance again.
Your providers at CTW like to think of Estrogen and Progesterone as sisters with different personalities. Estrogen is exciting, loud, provocative, and loves with all her heart (while protecting yours)! Progesterone is calm, steady, grounding, healing and gives you an inner glow.
Specific to your menstrual cycles, the first half of your cycle is ruled by Estrogen. She’s out there as a mover and a shaker, stimulating the ovaries to create and release an egg, encouraging the lining of your uterus to grow lush and large. After all of that hard work she *should* take a break and pass the baton to Progesterone.
Progesterone maintains that lining to welcome a potential very special guest… a fertilized egg. Hoping to turn this quick visit to a longer engagement, she’s sending out calming, grounding vibes and remaining present. But alas if this is not the way, with either no visitor or the wrong kind of visitor, she steps aside, the lining gives way, leaves the body in menstruation and the process starts again with big sis, E.
This is the healthy pattern in our child-bearing years, but as dysfunction becomes more common in our society, this may not be the “normal” pattern. We intentionally labeled Estrogen as the big sister, because she is the more dominant force between the two. If Estrogen is having too much of a good time, she is loud, lingering and can get kind of annoying. Progesterone is quiet and waiting off to the side, not able to provide her needed support and countermeasures.
Estrogen is produced not only by our ovaries, but also our adrenals and stored fat. Additionally it can enter our body in the form of fake estrogens, chemicals called xenoestrogens. These chemicals are estrogen wannabes and do as E does. They can be found lurking in our water, our food, even our personal care and household products. Gross.
When we want the party to be over, our body tries to reduce estrogen by breaking it down in our liver and sending it away via the toilet in a healthy bowel movement. Good bacteria in our gut are also trying to breakdown and escort out this fiery one, but only if good bacteria is in adequate amounts. Otherwise, non-beneficial bacteria act as estrogen promoters, sending out little enzyme agents to keep the party going.
Now let’s talk about the two times the female body will experience internal decline of progesterone beyond our monthly cycle. One, is very dramatic and the other, slow and steady.
During pregnancy, progesterone is sticking around and plays the lead role in maintaining a beautiful, lush environment for a thriving pregnancy. After pregnancy, progesterone dramatically decreases and that’s a big shift after 9 months! Mentally, we can experience this as postpartum mood changes like anxiety or depression.
A more subtle change over time is related to our bodies natural decline in progesterone production, which begins around age 35. From 35-50 years of age, Progesterone decreases 75%, while estrogen is only decreasing about 35%. And chances are, estrogen was already in abundance before this began.
So what might YOU be feeling if the sisters aren’t taking turns?
Again, we think of Estrogen as exciting, aka stimulating and things are more intense:
PMS
Breast tenderness
Pain with periods
Heavier and/or longer bleeding days
Irregular cycles
Mood swings
Brain fog
Sleep disturbances
What can YOU do to reduce estrogen?
At least one soft daily bowel movement is necessary! We are what we don’t poop!
You can help this lovely process and support healthy microbiome by eating prebiotic foods, rich in fiber and probiotic foods, rich in bacteria.
Eat Clean food! Limit processed foods, avoid artificial flavors and colors. Eat organic when you can, especially if it’s on the “Dirty Dozen” list, distributed annually by the Environmental Working Group.
Drink Clean water! Use a water filtration system, either countertop or whole home to reduce toxins.
Plastics….reduce your use! Plastic has softeners that are major Estrogen wannabes. Ditch those plastic water bottles, plastic food storage containers and microwaved plastic meals.
Check your makeup, personal hygiene products, cooking and cleaning supplies products for hidden xenoestrogens: parabens, phthalates, BPA, nonstick coatings.
Essential oils: rosemary
What can YOU do to increase progesterone?
Eat vitamin B rich foods! Salmon, leafy greens, organ meats, eggs, oysters, mussels…
Wild Yams are also progesterone enhancing foods, but not sweet potatoes.
Essential oils: thyme
Above just scratches the surface on two of the players involved in hormonal balance. While there are many things you can initiate on your own, there are also options for evaluation and support that a well-trained health care provider can offer. These tools and supports help you understand the needs of your unique system and implement successful, sustaining strategies to maintain your balance for many years to come!
We are honored to be your partners in health! Let us know if you would like to schedule an appointment to discuss your “Sister Act” personally by calling 919.999.0831.
Functional medicine is a science-based health care approach to assess, prevent and treat complex chronic disease.
![]() Learn More
Learn More
After a brief allergy test, you can begin sublingual immunotherapy (SLIT), or allergy drops under the tongue. No more allergy shots!
![]() Learn More
Learn More
Learn how to prepare for your visit and what to expect at your initial consultation and at your follow-up visits with our office.
![]() Learn More
Learn More